#omicron case india
Explore tagged Tumblr posts
Text
h3n2 | h3n2 virus | virus | corona virus | omicron virus | covid 19 | covid cases | covid news | covid news india
After Corona now H3N2 wreaks havoc, one person lost his life in Karnataka, you should also take these precautions It is being told that the old man suffering from the H3N2 virus died on March 1 itself and after his death, people in the surrounding areas of his village have also been investigated. Image Source: Pixabay Representational One person has died due to the H3N2 virus in…

View On WordPress
0 notes
Text
Old News (Published Nov, 2022)
Also preserved on our archive
Pro-Tip: All covid-19 strains are capable of immune escape from both vaccination and acquired immunity from infection! Mask up to prevent the spread of covid and further mutation toward immune escape!
By Alice Park
New lab data suggest that vaccines and prior infections may not offer enough protection against several new COVID-19 variants cropping up in the U.S. and around the world.
Dr. David Ho, director of Columbia University’s Aaron Diamond AIDS Research Center (ADARC), and his team reported the results from a set of studies at an ADARC symposium. They showed how well some of the latest variants—BQ.1, BQ.1.1, XBB, and XBB.1, which were all derived from Omicron—are evading both vaccine-derived and infection-derived immunity.
These new variants all have mutations in the region that binds to cells and infects them, which means that they’re highly transmissible, as prior Omicron variants were. BQ.1 is growing steadily in France, according to the public database of SARS-CoV-2 variants GISAID. By mid-November, European health officials expect the variant to account for 50% of cases in Europe, and to become the dominant strain in that region by early 2023. XBB is growing quickly in Singapore and India. Both variants have spawned new strains that have each picked up an additional mutation to create BQ.1.1 and XBB.1. As of early November, BQ.1 and BQ.1.1, combined, now make up about 35% of new cases in the U.S.
Other studies have found similar drops in antibody protection against BQ.1 among vaccinated people. But Ho’s group conducted what is likely the most comprehensive look to date at BQ.1, BQ.1.1, XBB, and XBB.1, and how existing immunity—from the original mRNA vaccines, the new Omicron boosters, and natural infections—stands up to them. Scientists took blood sera from 88 people in five groups (below) and exposed it to the four variants in the lab. Here’s what they found:
Fully vaccinated and once-boosted people (three total shots of the original mRNA vaccines) had 37- and 55-fold lower neutralization against BQ.1 and BQ.1.1, respectively, than they did against the original SARS-CoV-2 virus, and about 70-fold lower neutralization against XBB and XBB.1. Fully vaccinated and twice-boosted people (four total shots of the original mRNA vaccines) had 43- and 81-fold lower neutralization against BQ.1 and BQ.1.1, respectively, than they did against the original virus, and 145- and 155-fold lower neutralization against XBB and XBB.1, respectively. Fully vaccinated and twice-boosted people (three shots of the original vaccine plus one Omicron booster) had 24- and 41-fold lower neutralization against BQ.1 and BQ.1.1, respectively, than they did against the original virus, and 66- and 85-fold lower neutralization against XBB and XBB.1, respectively. Fully vaccinated people who had received the original booster and who had been infected with BA.2 had 20- and 29-fold lower neutralization against BQ.1 and BQ.1.1, respectively, than they did against the original virus, and 103- and 135-fold lower neutralization against XBB and XBB.1, respectively. Fully vaccinated people who had received the original booster and who had been infected with BA.4 or BA.5 had 13- and 31-fold lower neutralization against BQ.1 and BQ.1.1, respectively, than they did against the original virus, and 86- and 96-fold lower neutralization against XBB and XBB.1, respectively.
The results show that people who had been infected with BA.2, BA.4, or BA.5 generally experienced the smallest drop in neutralizing antibody levels against against BQ.1 and BQ.1.1. But people who had three doses of the original vaccine and one Omicron booster produced only slightly better neutralizing antibody protection against XBB and XBB.1 than those who received three doses of the original vaccine. Public-health experts say that while vaccines may wane in efficacy against newer variants, they continue to protect people from severe COVID-19. There is early evidence that vaccine-induced immunity may also produce a broader range of virus-fighting antibodies over time.
Read More: BQ.1, BQ.1.1, BF.7, and XBB: Why New COVID-19 Variants Have Such Confusing Names
Still, these results are a reminder that vaccines and drug treatments need to evolve with the virus. “These new variants are extremely good at evading our antibodies and are very likely to compromise the efficacy of our vaccines,” says Ho. They may also dodge the available antibody-based treatments for COVID-19, he says. The National Institutes of Health’s COVID-19 Treatment Guidelines currently only include one monoclonal antibody therapy, bebtelovimab, because the virus has evaded all of the previously authorized antibody treatments. But in an October update, NIH scientists acknowledged that the “subvariants BQ.1 and BQ.1.1 are likely to be resistant to bebtelovimab.” The drug is therefore only recommended if people either can’t take the antiviral drugs Paxlovid or remdesivir, or if these medications aren’t available. The virus can evade these treatments as well, but they remain the first line of defense against severe SARS-CoV-2.
The good news is that in places where these variants are spreading, they do not seem to be linked to more severe COVID-19 disease—measured by hospitalizations and deaths—than other Omicron iterations. Still, public-health experts say a spike in infections could still strain health resources, especially as other respiratory infections, including influenza and RSV, also gain momentum. The combination of several circulating infectious diseases could mean more illness overall, and, in turn, more people who might experience severe disease and require intensive medical care.
The rise of BQ.1, BQ.1.1, XBB, and XBB.1 points to the fact that when it comes to immunity, the virus may always be one step ahead, especially with respect to vaccines. “I would start to make these vaccines, and start to test them in animals,” says Ho. Even if those efforts began now, it’s possible they may still lag behind the virus and the new mutations it continues to gain. That’s why researchers are working on developing vaccines that would be more universally applicable to a range of different coronaviruses, which could shorten the amount of time it takes to build up a vaccinated population’s immunity.
#mask up#covid#pandemic#wear a mask#public health#covid 19#wear a respirator#still coviding#coronavirus#sars cov 2#covid pandemic#covidー19#covid conscious#covid is airborne#covid isn't over#covid19
19 notes
·
View notes
Text
Zero, Negative, and Infinite Numbers in Antiquity
With the advent of accounting, numbers became more important to people of the Bronze Age and into the Iron Age. Numbers grew into a thing of philosophy as much as they were of accounting and geometry. Number systems were developed, based on systems of 10, 20, or even 60, depending on the culture, but numbers having a value based on where in the number they appear, such as the value of 4 being different in 4356, 43, and 354, was something that came along later. This is something we take for granted now, but wasn't developed until the Hindu people of India. The biggest development that allowed for a positional system of numbers is 0.
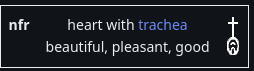
Zero shows up in some ways before the Hindu-Arabic numeral system was formalized. The Ancient Egyptians used a symbol called 'nfr' to symbolize when the amount received by pharaoh was equal to what was distributed, but they did not use a positional system when writing other numbers. The Babylonians also didn't use a positional number system, though they might use three hooks, or later two slants, as punctuation marks between between numbers like we use zero now, but they were never used alone or at the end of a number, showing that the concept wasn't fully developed yet.
By Miranche - Own work, CC BY-SA 4.0, https://commons.wikimedia.org/w/index.php?curid=55976282
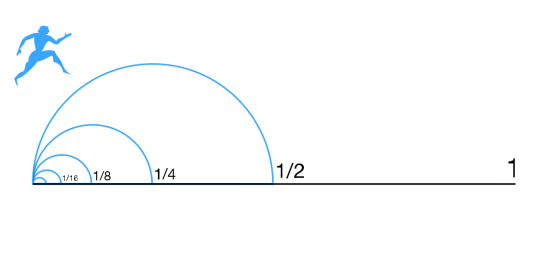
The ancient Greeks seemed to be philosophically opposed to zero while also needing to use it for their astronomy. They used lower case omicron (ό) initially in place of the punctuation marks that the Babylonians used. The quantity of zero led to the philosophical question 'how can not being be?', on which the paradoxes of Zeno of Elea rest (one of which being 'that which is locomotion must arrive at the half-way stage before it arrives at the goal').
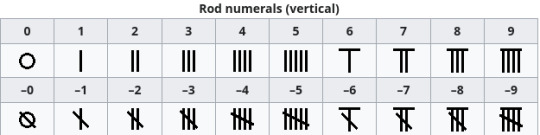
The ancient Chinese used a counting rod system that allowed positive and negative numbers depending on how exactly the numbers were written, but treated zero itself as a vacant place, lending the system a type of positional set up, but without having a zero or null concept. At some point prior to CE 1274, the symbol 〇 as the placeholder and was probably borrowed from the Indian people.
By National Geographic - National Geographic [1]. Non creative image of a 2D artifact from the 3-4th century CE., Public Domain, https://commons.wikimedia.org/w/index.php?curid=73315832
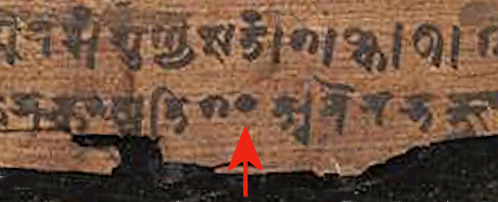
In India, a black dot was used as a symbol for zero, which gradually became hollow. It was fully recognized as a number as far back as CE 224, though Pingala, a Sanskrit scholar who lived around the 2nd or 3rd century BCE, created a type of notation similar to Morse code with long and short sylables and included a zero, using the word Śūnyatā शून���यता to represent zero. The word is generally translated as 'insubstance' or 'nothingness'.
Negative numbers are a part of accounting, so they existed from the beginning of the idea of counting. The only known group of peoples to have specific notation for them, though, are the ancient Chinese with their counting rod system.
By Nevit Dilmen - Own work, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=4182698
In ancient cultures, infinity wasn't a number, but an idea to be explored through philosophy. The earliest record we have of this discussion is Anaximander, who lived from about 610-546 BCE, who called it apeiron ἄπειρον, which is translated as 'unlimited, boundless, indefinite'. He considered this to be the basis of reality. Anaxagoras, who lived from about 500-428 BCE, believed that the universe had the capacity to be infinitely divided (leading to the idea of atoms). Aristotle (384-322 BCE) rejected the idea that infinity was a real thing and could only be an idea. Aristotle's ideas were not widely disputed until the Enlightenment.
By I, Tó campos1, CC BY-SA 3.0, https://commons.wikimedia.org/w/index.php?curid=2304574
Early Indian thinking on infinity was written into the Jain upanga Agamas जैन साहित्य around 400 BCE. There it is held that numbers can be divided into three groups: enumerable (lowest, intermediate, highest), innumerable (nearly innumerable, truly innumerable, innumerably innumerable), and infinite (nearly infinite, truly infinite, infinitely infinite). They were the first group to recognize that not all infinites are the same, which corresponds with the modern mathematical thinking. Infinite length, infinite area, and infinite volume are all infinites, but not the same infinite.
#numbers#ancient egypt#hindu numbers#infinity#negative numbers#zero#mathematics#math history#maths history
2 notes
·
View notes
Text
[...]
Cases aren't the only thing dropping either — so is surveillance of the virus. We're doing less testing and less sequencing of SARS-CoV-2 genetics.
Given all this, the question begs to be asked: Are we letting our guard down while waving the Mission Accomplished flag?
When asked if there is adequate surveillance for new variants happening, Dr. Margaret Harris, a spokesperson for the World Health Organization (WHO), flatly said no.
"Current trends in reported COVID-19 cases are underestimates of the true number of global infections and reinfections as shown by prevalence surveys," Harris told Salon in an email. "This is partly due to the reduction in testing and delays in reporting in many countries. Reduction in testing means a reduction in genetic sequencing, as you need to find the virus first in order to sequence it."
"We continually call on member states to maintain strong testing and sequencing in order to identify new variants but also to understand the level of SARS-CoV-2 transmission going on in their populations," Harris continued. "This virus remains unstable — it has not settled into a predictable pattern, which means surveillance systems need to be sensitive to pick up the early signs of another surge."
XBB.1.5, nicknamed by some as "Kraken," is thus far the dominant variant for most of 2023, with estimated cases of Kraken exceeding 70 percent since the week of Feb 11. It has far eclipsed the BQ.1 and BQ.1.1 variants. Meanwhile BA.2 and BA.5, the two variants that dominated case counts for most of 2022, have all but disappeared.
According to the latest CDC variant tracking data, the only other variants really circulating in the U.S. are XBB.1.5's offspring: XBB.1.9 and XBB.1.5.1. Meanwhile, XBB.1.16 is spreading rapidly in India and could eventually make its way to North America. Notably, XBB was first detected in Singapore before its offspring made the jump across the Pacific, though XBB.1.5 was first detected in the U.S. and likely originated in the Northeast.
All these names may sound like gobbledygook to most non-experts — and there is a reason it's so confusing. When variants of the virus mutated and evolved into new strains with significant advantages over old lineages, the WHO began giving these "variants of concern" names from the Greek alphabet. Hence, variants like delta and gamma made headlines when they emerged and began to spread — but the WHO has yet to assign any variants a new Greek name since omicron surged in late 2021. Instead, we have this alphabet soup of named variants, all of which are technically different sub-strains of omicron.
Even a minor variation in a virus' genetics can equate to a huge difference in how well immunity from vaccines and previous infections can stop them. If the virus evolves some kind of advantage — as viruses are prone to do and just as SARS-CoV-2 has done many times throughout the pandemic — another surge is not out of the question.
In mid-March, the WHO updated their definition of what makes COVID variants threatening and currently classifies XBB.1.5 as a "variant of interest," which means it is seen as less threatening than previous variants of concern.
Nonetheless, some virologists have argued that XBB and its close relatives are so genetically different from the very first strain of SARS-CoV-2 that it should technically be renamed a new virus, SARS-CoV-3.
"XBB.1.5 does show a growth advantage and a higher immune escape capacity, but evidence from multiple countries does not suggest that XBB and XBB.1.5 are associated with increased severity or mortality," Harris said. "In countries where the variant has driven an increase in cases, the waves are significantly smaller in scale compared to previous waves."
That's good news, but as the virus bounces between hemispheres, it may gain new mutations that allow it to infect more effectively or evade immunity. Some of our treatments, but not all, have stopped working against XBB strains. Monoclonal antibodies don't stop it, but antiviral drugs like Paxlovid and bivalent booster vaccines are still very effective.
But the combined lack of public interest in the pandemic, exemplified in victory marches from political leadership, has led to a shrinking pool of data on COVID as there is less funding afforded to tracking and research. As we've seen in previous surges, the situation can change without warning. The situation is made worse by wild animals that harbor COVID, a viral reservoir that could spill back to humanity if given the opportunity.
"The level of genomic surveillance has been dropping off, and there are also indications that funding for wastewater monitoring will be ending in some places," Dr. T. Ryan Gregory, an evolutionary and genome biologist at the University of Guelph in Canada, told Salon in an email. "We have far less information than we used to, which hampers the ability to detect and track new variants. It's also worth noting that India and China include about one-third of the world's population, and we have very little information on variants there."
While overall trends are down, many people would be especially vulnerable to a COVID infection right now, according to Dr. Rajendram Rajnarayanan, an assistant dean of research and associate professor at the New York Institute of Technology campus in Jonesboro, Arkansas.
"Very few of us have had the bivalent booster, so in terms of protection, we are kind of vulnerable," Rajnarayanan told Salon. He noted that COVID is still a serious, life-threatening disease for immunocompromised people and those over 70. Most people who got bivalent booster shots — if they did so at all — received the jab in the fall. By now, that immunity has likely waned and there hasn't been much communication about when or if a new booster will come out later this year. According to NPR, the Food and Drug Administration has said it will allow some people over the age of 65 to get a second bivalent booster, but it hasn't been officially announced yet.
So while infections are trending downward, immunity is as well. In the past, major gaps in immunity have been followed by major surges, such as with delta and omicron.
"When there is a big pause, and some new variant comes, we are not really protected. But when there are repeated waves, the previous wave usually protects the next wave." Rajnarayanan said. "Every time the variant goes down, something goes up later on. Just the gap between the two peaks has changed."
Despite the unpredictability of SARS-CoV-2, the strategy for fighting it hasn't changed. Masking in public, improving indoor ventilation, testing when appropriate, staying home when sick and keeping up with vaccines when possible are good strategies for keeping the virus at bay. But overall, it's not enough to say the emergency is over. We need to be strategic and keep a close eye on the evolution of COVID as well.
"People have changed, our approaches have changed, and we don't need any modern approaches to defeat this virus," Rajnarayanan said. "We know how to do this . . . we have to do it collectively. That's all there is to it."
9 notes
·
View notes
Text
21 cases of Covid-19 subvariant JN. 1 detected in India, authorities on high alert
With the fresh cases of coronavirus subvariant JN.1 emerging in India, Indian authorities have been on high alert. The subvariant JN. 1 is being investigated by the scientific community as the authorities work on curbing its spread already. As per NITI Aayog member (health) Dr V K Paul, as of now, 21 cases of COVID-19 JN.1 sub-variant have been detected in the country. The Indian Council of Medical Research (ICMR) is focused on the genome sequencing of the variant.
Out of the 21 cases, 19 cases have been detected in Goa while Kerala and Maharashtra have recorded one each.
First found in late 2023, the JN.1 (BA.2.86.1.1) variant of COVID-19 is a descendant of the BA.2.86 lineage (Pirola) of SARS-CoV-2. The BA.2.86 lineage (Pirola) first emerged in August 2023 and showed more than 30 mutations in the spike (5) protein unlike the SARS-CoV-2 Omicron XBB lineages. The mutations make the variant highly risky with a high potential for immune evasion.
The JN.1 subvariant has been classified as a variant of interest by the World Health Organization.
Head of Pulmonary Medicine at Safdarjung Hospital, Dr. Rohit Kumar said, “COVID is an RNA virus that changes its form from time to time, and new variants of it emerge. And now a new variant has emerged, which has been named JN.1. However, not a single case has come to light in the capital, Delhi yet.”
"We are on alert, keeping an eye on the Corona cases. Testing of patients is also being done, and the patients who are coming positive are also being sent for genome sequencing. So that new variants can also be detected, but till now no case of new variants has been reported in Delhi," Dr Kumar said.
"If there is a sore throat, cough, cold, chest pain, or difficulty breathing, consult the doctor immediately. Especially those already suffering from respiratory diseases and asthma patients need to take special care. The doctor mentioned that during this season, individuals with serious diseases should be more careful, as those dying due to Covid often have pre-existing serious conditions such as heart disease and diabetes," he added.
For more COVID-19 news India in Hindi, subscribe to our newsletter.
#werindia#top news stories#leading india news source#top news headlines#top news of the day#latest national news#national news#coronavirus#covid19#JN.1 Covid variant
0 notes
Text
vimeo
Hiranandani Hospital Powai News - Omicron Breakthrough Infections in Mumbai - Understanding the Importance of Booster Doses
The Dr Sujit Chatterjee Hiranandani Hospital Powai provided an example. He explained that since the influenza virus changes frequently so the vaccine is reformulated every year. The anti-Covid vaccines will also be not effective since they won't be exclusive to the current strain of the virus, called Omicron. In the report by Dr Sujit Chatterjee Hiranandani Hospital Latest News, India had 358 Omicron cases on December 24, evening, distributed across 17 states including Maharashtra being the biggest number with at 108.
Learn More at https://www.hiranandanihospital.org/
#hiranandani hospital kidney transplant#hiranandani hospital kidney#hiranandani hospital powai news#hiranandani hospital reviews#hiranandani hospital powai covid#hiranandani powai hospital#hiranandani hospital#hiranandani hospital kidney care#hiranandani hospital powai#hiranandani hospital kidney tranplant#Vimeo
0 notes
Text
Deciphering the Complexities of COVID-19 Variants
Introduction:
The global COVID-19 pandemic has posed an unprecedented challenge to humanity. As the virus continues its relentless spread, it constantly evolves through mutations, giving rise to an array of variants. In this in-depth journey, we will embark on a thorough exploration of the intricate realm of COVID-19 variants to equip you with the indispensable knowledge you need.
1. Unraveling the Intricate World of COVID-19 Variants:
COVID-19 variants are akin to unique adaptations of the SARS-CoV-2 virus, each sculpted by genetic mutations. These genetic transformations can lead to substantial changes in the virus's characteristics, influencing its transmissibility, disease severity, and resistance to immunity. Think of these variants as distinct "iterations" of the same virus, each bearing its genetic signature.
2. An In-Depth Exploration of Prominent COVID-19 Variants:
Alpha (B.1.1.7): First detected in the United Kingdom, the Alpha variant gained worldwide attention due to its heightened transmissibility. However, it didn't necessarily translate into more severe illness or increased fatality rates.
Beta (B.1.351): Originating in South Africa, the Beta variant raised concerns about its potential resistance to immunity, including vaccine-induced immunity. Researchers maintained a vigilant watch over its behavior.
Delta (B.1.617.2): The Delta variant, initially identified in India, has played a pivotal role in the pandemic. Its extraordinary transmissibility led to surges in cases worldwide, resulting in increased hospitalizations and posing challenges to containment efforts.
Omicron (B.1.1.529): Omicron made global headlines due to its numerous mutations in the spike protein, the primary target of most COVID-19 vaccines. Scientists are actively researching its transmissibility, severity, and vaccine efficacy, given its potential risk.
3. Understanding the Genesis of Variants:
Why Do They Emerge? Variants are an inherent facet of a virus's life cycle. As the virus replicates and spreads, genetic changes occur. While many of these changes are random, some provide advantages to the virus. For instance, mutations that enhance transmissibility help the virus spread more efficiently from person to person, ultimately increasing its prevalence.
4. Assessing the Impact of Variants on Vaccines:
A major concern regarding COVID-19 variants revolves around their impact on vaccine effectiveness. Vaccine manufacturers and researchers vigilantly monitor these variants. While some variants may marginally reduce vaccine effectiveness, it is crucial to understand that vaccines continue to offer robust protection against severe illness, hospitalization, and death. Even when a variant affects vaccine efficacy, vaccines remain potent in mitigating the virus's impact.
In response to the emergence of variants, booster shots have been recommended to enhance immunity, especially against newer and more challenging variants like Delta and Omicron. These booster doses bolster the body's immune response, providing additional layers of protection.
5. The Pivotal Role of Public Health Measures:
Irrespective of the variants that emerge, public health measures remain crucial for controlling the spread of COVID-19. These measures encompass:
Mask-Wearing: Consistently don masks in crowded or indoor settings, especially in regions with high transmission rates.
Social Distancing: Maintain physical distance from others, particularly during close social interactions.
Hand Hygiene: Practice regular handwashing with soap and water or use hand sanitizers.
Vaccination: If eligible, get vaccinated and adhere to guidance on booster shots when provided.
Testing and Isolation: Undergo testing if you display symptoms or have been exposed to a COVID-19-positive individual. Prompt isolation upon receiving a positive result is essential to curb further transmission.
These measures not only safeguard individual health but also act as barriers against the emergence of new variants.
Summary:
COVID-19 variants are an intrinsic part of the virus's evolution. Scientists diligently explore their characteristics and potential impact on public health. In this ever-evolving landscape, vaccination and adherence to public health measures remain our most unwavering allies in the battle against the pandemic. Staying informed and heeding guidelines from reputable health authorities, such as the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC), are essential actions to safeguard ourselves and our communities.
0 notes
Text
Unmasking the Complexity of COVID-19 Variants
Introduction:
The global COVID-19 pandemic has posed an unprecedented challenge to humanity. As the virus continues its relentless spread, it constantly evolves through mutations, giving rise to an array of variants. In this in-depth journey, we will embark on a thorough exploration of the intricate realm of COVID-19 variants to equip you with the indispensable knowledge you need.
1. Unraveling the Intricate World of COVID-19 Variants:

COVID-19 variants are akin to unique adaptations of the SARS-CoV-2 virus, each sculpted by genetic mutations. These genetic transformations can lead to substantial changes in the virus's characteristics, influencing its transmissibility, disease severity, and resistance to immunity. Think of these variants as distinct "iterations" of the same virus, each bearing its genetic signature.
2. An In-Depth Exploration of Prominent COVID-19 Variants:
Alpha (B.1.1.7): First detected in the United Kingdom, the Alpha variant gained worldwide attention due to its heightened transmissibility. However, it didn't necessarily translate into more severe illness or increased fatality rates.
Beta (B.1.351): Originating in South Africa, the Beta variant raised concerns about its potential resistance to immunity, including vaccine-induced immunity. Researchers maintained a vigilant watch over its behavior.
Delta (B.1.617.2): The Delta variant, initially identified in India, has played a pivotal role in the pandemic. Its extraordinary transmissibility led to surges in cases worldwide, resulting in increased hospitalizations and posing challenges to containment efforts.
Omicron (B.1.1.529): Omicron made global headlines due to its numerous mutations in the spike protein, the primary target of most COVID-19 vaccines. Scientists are actively researching its transmissibility, severity, and vaccine efficacy, given its potential risk.
3. Understanding the Genesis of Variants:
Why Do They Emerge? Variants are an inherent facet of a virus's life cycle. As the virus replicates and spreads, genetic changes occur. While many of these changes are random, some provide advantages to the virus. For instance, mutations that enhance transmissibility help the virus spread more efficiently from person to person, ultimately increasing its prevalence.
4. Assessing the Impact of Variants on Vaccines:

A major concern regarding COVID-19 variants revolves around their impact on vaccine effectiveness. Vaccine manufacturers and researchers vigilantly monitor these variants. While some variants may marginally reduce vaccine effectiveness, it is crucial to understand that vaccines continue to offer robust protection against severe illness, hospitalization, and death. Even when a variant affects vaccine efficacy, vaccines remain potent in mitigating the virus's impact.
In response to the emergence of variants, booster shots have been recommended to enhance immunity, especially against newer and more challenging variants like Delta and Omicron. These booster doses bolster the body's immune response, providing additional layers of protection.
5. The Pivotal Role of Public Health Measures:
Irrespective of the variants that emerge, public health measures remain crucial for controlling the spread of COVID-19. These measures encompass:
Mask-Wearing: Consistently don masks in crowded or indoor settings, especially in regions with high transmission rates.
Social Distancing: Maintain physical distance from others, particularly during close social interactions.
Hand Hygiene: Practice regular handwashing with soap and water or use hand sanitizers.
Vaccination: If eligible, get vaccinated and adhere to guidance on booster shots when provided.
Testing and Isolation: Undergo testing if you display symptoms or have been exposed to a COVID-19-positive individual. Prompt isolation upon receiving a positive result is essential to curb further transmission.
These measures not only safeguard individual health but also act as barriers against the emergence of new variants.
Summary:
COVID-19 variants are an intrinsic part of the virus's evolution. Scientists diligently explore their characteristics and potential impact on public health. In this ever-evolving landscape, vaccination and adherence to public health measures remain our most unwavering allies in the battle against the pandemic. Staying informed and heeding guidelines from reputable health authorities, such as the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC), are essential actions to safeguard ourselves and our communities.
0 notes
Text
Why Biden’s premature COVID ending could help it surge - Published Sept 23, 2022
Two years out from the publication of this article, and we can really see how true these warnings were. Why does the mainstream media and DNC refuse to do anything about forever covid?
This week, President Biden said what millions of Americans have been hoping to hear since the spring of 2020: “The pandemic is over.”
I understand the impulse to close the book and move on. But I am deeply concerned that this declaration is not only premature but also dangerous.
The SARS-CoV-2 virus has shown us, again and again, the danger of hubris. Think of the lethal impact of the omicron virus last winter, just when we were so grateful that the delta wave had ebbed. Think of the deadly surges this summer, just when we were planning our long-delayed vacations. This is a virus that has humbled us too often. We must approach it with humility.
This declaration has many damaging effects: As others have noted, it will now be even harder to persuade Americans to get the new bivalent boosters. It’ll be tougher to persuade Congress to fund essential COVID responses. And it will be nearly impossible for local officials to impose new indoor mask requirements should another surge arrive.
To be sure, Biden did acknowledge in his “60 Minutes” interview that “we still have a problem with COVID” and added that “we’re still doing a lot of work on it.” But he sandwiched that message between two flat declarations that the pandemic is over. Those are the soundbites that have reverberated most loudly, and they are decidedly unhelpful.
Dr. Tom Frieden, former director of the Centers for Disease Control and Prevention, has spoken often about how the U.S. has lurched from a cycle of panic to neglect when it comes to public health. Many of us in the field had hoped that the COVID-19 pandemic would break that cycle — a sliver of silver lining amid all the grief.
We had hoped that policymakers and voters alike would understand how essential it is to upgrade our data infrastructure, stockpile essential medicine and equipment, invest in preventive care for vulnerable populations, restructure our emergency response agencies and support an infusion of public health workers at the local and state levels. Surely, COVID would be the spur needed to finally bump U.S. spending on public health to more than 3 cents on the health care dollar.
By declaring the pandemic over when we are still very much in the thick of the fight, President Biden is undercutting that message.
Let’s look at where we are right now. The U.S. is still reporting close to 60,000 cases and 400 deaths each day. Millions are struggling with long COVID; by some estimates, this often debilitating condition is keeping 4 million adults out of work. Those at work may have less flexibility: Major companies are ending work-from-home policies and Starbucks announced this week that it will no longer give employees paid time off to isolate or get vaccinated. Biden’s remarks will only accelerate that trend.
Meanwhile, only 67 percent of Americans are vaccinated and only half of them have been boosted. While many of the remaining have some immunity from infection, the death toll makes clear that large swaths of the population remain highly vulnerable. And of course, new variants continue to emerge; right now, all eyes are on BA.2.75.2, a mutation of the omicron variant that is notably better at evading antibodies acquired from vaccination or prior infection and is spreading rapidly in India.
Declaring the pandemic over at this stage is tantamount to accepting all this misery as background noise.
And if we accept the status quo as background noise — rather than the urgent and immediate threat it represents — it’s nearly impossible to make the case that we need to do more as a society to protect the vulnerable, respond to surges, or prepare for future crises.
The Biden administration has made significant strides on COVID. It made tests, vaccines and treatments widely available across the country, which improved outcomes and saved lives. The vast majority of Americans feel we’re in a better place than at this time last year and many have returned, at least in large part, to normal activities.
It is an appropriate moment for our leaders to turn the page away from our wartime footing and begin a sober discussion about the next steps: the risks that remain, the importance of responding quickly to local surges, the value of supporting the Global South in building their own vaccine infrastructure — and the critical need to rebuild the battered and woefully outdated public health infrastructure in the U.S.
It is not the moment to declare victory.
John M. Barry, author of “The Great Influenza: The Story of the Deadliest Pandemic in History” has a stark warning from history. He writes that the world had largely moved on from the 1918 influenza pandemic when a fourth wave struck in 1920. By then, the U.S. had plenty of natural immunity from prior infection. Still, the virus spread ruthlessly. Public officials failed to respond. They, like the public, wanted the pandemic to be over — so the virus rolled on unchecked. In some cities, the death toll in 1920 exceeded the toll of the huge second wave.
We should not make the same mistake now. With humility as our watchword, we can move to the next chapter without closing the book. That is the way forward.
Michelle A. Williams is dean of the faculty of the Harvard T.H. Chan School of Public Health.
#covid#mask up#pandemic#covid 19#wear a mask#coronavirus#sars cov 2#public health#still coviding#wear a respirator#us politics#joe biden#democratic party
16 notes
·
View notes
Text
Demystifying the Complexities of COVID-19 Mutations: A Comprehensive Exploration
Introduction:
The global COVID-19 pandemic has posed an unprecedented challenge to humanity. As the virus continues its relentless spread, it constantly evolves through mutations, giving rise to an array of variants. In this in-depth journey, we will embark on a thorough exploration of the intricate realm of COVID-19 variants to equip you with the indispensable knowledge you need.
1. Unraveling the Intricate World of COVID-19 Variants:
COVID-19 variants are akin to unique adaptations of the SARS-CoV-2 virus, each sculpted by genetic mutations. These genetic transformations can lead to substantial changes in the virus's characteristics, influencing its transmissibility, disease severity, and resistance to immunity. Think of these variants as distinct "iterations" of the same virus, each bearing its genetic signature.
2. An In-Depth Exploration of Prominent COVID-19 Variants:
Alpha (B.1.1.7): First detected in the United Kingdom, the Alpha variant gained worldwide attention due to its heightened transmissibility. However, it didn't necessarily translate into more severe illness or increased fatality rates.
Beta (B.1.351): Originating in South Africa, the Beta variant raised concerns about its potential resistance to immunity, including vaccine-induced immunity. Researchers maintained a vigilant watch over its behavior.
Delta (B.1.617.2): The Delta variant, initially identified in India, has played a pivotal role in the pandemic. Its extraordinary transmissibility led to surges in cases worldwide, resulting in increased hospitalizations and posing challenges to containment efforts.
Omicron (B.1.1.529): Omicron made global headlines due to its numerous mutations in the spike protein, the primary target of most COVID-19 vaccines. Scientists are actively researching its transmissibility, severity, and vaccine efficacy, given its potential risk.
3. Understanding the Genesis of Variants:
Why Do They Emerge? Variants are an inherent facet of a virus's life cycle. As the virus replicates and spreads, genetic changes occur. While many of these changes are random, some provide advantages to the virus. For instance, mutations that enhance transmissibility help the virus spread more efficiently from person to person, ultimately increasing its prevalence.
4. Assessing the Impact of Variants on Vaccines:

A major concern regarding COVID-19 variants revolves around their impact on vaccine effectiveness. Vaccine manufacturers and researchers vigilantly monitor these variants. While some variants may marginally reduce vaccine effectiveness, it is crucial to understand that vaccines continue to offer robust protection against severe illness, hospitalization, and death. Even when a variant affects vaccine efficacy, vaccines remain potent in mitigating the virus's impact.
In response to the emergence of variants, booster shots have been recommended to enhance immunity, especially against newer and more challenging variants like Delta and Omicron. These booster doses bolster the body's immune response, providing additional layers of protection.
5. The Pivotal Role of Public Health Measures:
Irrespective of the variants that emerge, public health measures remain crucial for controlling the spread of COVID-19. These measures encompass:
Mask-Wearing: Consistently don masks in crowded or indoor settings, especially in regions with high transmission rates.
Social Distancing: Maintain physical distance from others, particularly during close social interactions.
Hand Hygiene: Practice regular handwashing with soap and water or use hand sanitizers.
Vaccination: If eligible, get vaccinated and adhere to guidance on booster shots when provided.
Testing and Isolation: Undergo testing if you display symptoms or have been exposed to a COVID-19-positive individual. Prompt isolation upon receiving a positive result is essential to curb further transmission.
These measures not only safeguard individual health but also act as barriers against the emergence of new variants.
Summary:
COVID-19 variants are an intrinsic part of the virus's evolution. Scientists diligently explore their characteristics and potential impact on public health. In this ever-evolving landscape, vaccination and adherence to public health measures remain our most unwavering allies in the battle against the pandemic. Staying informed and heeding guidelines from reputable health authorities, such as the World Health Organization (WHO) and the Centers for Disease Control and Prevention (CDC), are essential actions to safeguard ourselves and our communities.
0 notes
Text
RAJKOT UPDATE NEWS THIS SYMPTOM OF OMICRON APPEARS ONLY ON THE SKIN
The Omicron variation of SARS-CoV-2 has been related to a number of novel scientific displays, together with cutaneous manifestations because the number one or sole symptom in a few individuals. This article reviews the modern-day evidence regarding these cutaneous manifestations, the underlying pathophysiological mechanisms, and capability implications for prognosis, management, and public fitness measures. More on rajkot update news this symptom of omicron appears simplest at the skin is described underneath.
The Omicron variant of SARS-CoV-2, first diagnosed in November 2021, has established giant changes in transmission dynamics and scientific features compared to earlier strains of the virus. While breathing signs and symptoms stay predominant, a subset of patients has been determined to provide with cutaneous manifestations because the number one or sole symptom. This article goals to provide a complete overview of the modern-day literature on cutaneous manifestations related to the Omicron variation, which includes potential mechanisms and implications for scientific exercise. You have to acquire facts on omicron cases in India.
Methods A literature seek became performed the usage of the PubMed, EMBASE, and Cochrane Library databases to become aware of applicable research published up to April 2023. Articles have been included in the event that they focused on cutaneous manifestations in sufferers with confirmed Omicron variant contamination, and were published in English. Data have been extracted and synthesized narratively. @ Read More This Symptom Of Omicron, Appears Only On The Skin
1 note
·
View note
Text

Arcturus' is a spin-off of the Omicron variant and is believed to be the most contagious variant yet. A new Covid😷 variant which has ripped through India and seen the country bring back face masks has been detected in the UK with 50 cases now reported.
The new Covid variant called 'Arcturus', which has been wreaking havoc in India, has already been detected in Britain. Hospitals in India are on red alert, with some states reintroducing compulsory face masks to curb the rocketing infection rates, which have increased 13-fold in the past month.
While the rise in cases is a cause for concern, it is still much lower than the devastating wave of cases that India experienced in 2021 during the Delta wave. Scientists do not expect the variant, scientifically known as XBB.1.16, to be more lethal than other types of Covid currently circulating. The UK Health and Security Agency had reported in its final variant report issued last month that the 'Arcturus' variant had already been detected in the UK. Separate data from variant trackers indicate that the UK has sequenced nearly 50 samples of 'Arcturus'.
'Arcturus' is a spin-off strain of Omicron, similar to the Kraken variant (XBB.1.5), and has been detected in 22 countries since it emerged in March. The largest outbreak by far has been in India, where it has led to a surge in cases with infections increasing 13-fold within the last month. This has prompted health authorities in India to run hospital drills and reintroduce mask mandates in some areas.
'Arcturus' has mutations on its spike protein that the World Health Organization (WHO) says could increase its ability to infect people and trigger disease. Japanese researchers have suggested that it is 1.2 times more infectious than the already highly transmissible Kraken variant. However, there is no evidence to suggest that it increases the severity of the disease. Early results suggest that 'Arcturus' does not have any increased ability to evade protection from vaccines compared to other Omicron spin-offs.
Officials in India believe that the 'Arcturus' variant is driving the latest wave of Covid cases in the country. The Ministry of Health in India has conducted mock drills to assess the preparedness of hospitals for a potential influx of patients, and some states have reintroduced face mask mandates in public settings for the first time in over a year. As of April 12, there were 40,215 active Covid cases in India, an increase of 3,122 in just one day. Separate data from the Oxford University-run platform Our World in Data show that new daily cases reached 3,108 on April 4, up from 242 one month earlier.
0 notes
Text
‘Arcturus,’ or XBB.1.16 #COVID19 variant, the most transmissible yet and sweeping India, is now in the US, says CDC. It is estimated to be behind 7% of COVID cases in the country. What it means for the future of the pandemic?
#Arcturus #XBB116 #Omicron
instagram
0 notes