#Medical Records Data Entry Services
Explore tagged Tumblr posts
Text
[“As computer programs determine how many patients can be profitably squeezed into a day, doctors become tools. Then the actual machines march triumphantly into the wards.
Nurses are now separated from patients by computers on wheels that roll everywhere with them: their bossy robot taskmasters. When you first see a nurse, she or he will likely have eyes on the screen rather than on you. This has dreadful consequences for your treatment, since you become a checklist rather than a person. If you are having a problem unrelated to what is on the screen, some nurses will have a hard time gathering themselves and paying attention. For example, after my first liver procedure my liver drain was improperly attached. This was a serious problem that was easily reparable. Yet although I tried for four days to draw attention to it, I could not get through. It was not on the lists. And so I had a second liver procedure.
When I read my own medical record, I was struck by how often doctors wrote what was convenient rather than what was true. It’s hard to blame them: they are locked in a terrible record-keeping system that sucks away their time and our money. When doctors enter their records, their hands are guided by the possible entries in the digital system, which are arranged to maximize revenue. The electronic medical record offers none of the research benefits that we might expect from its name; it is electronic in the same sense that a credit card reader or an ATM is electronic. It is of little help in assembling data that might be useful for doctors and patients.
During the coronavirus pandemic, doctors could not use it to communicate about symptoms and treatments. As one doctor explained, “Notes are used to bill, determine level of service, and document it rather than their intended purpose, which was to convey our observations, assessment, and plan. Our important work has been co-opted by billing.” Doctors hate all of this.
Doctors of an older generation say that things were better in their time—and, what is more worthy of note, younger doctors agree with them. Doctors feel crushed by their many masters and miss the authority that they used to enjoy, or that they anticipated that they would enjoy when they decided to go to medical school. Young people go to medical school for good reasons, then find their sense of mission exploited by their bosses. Pressured to see as many patients as possible, they come to feel like cogs in a machine. Hassled constantly by companies that seek to pry open every aspect of medical practice for profit, they find it hard to remember the nobility of their calling. Tormented by electronic records that take as much time as patient care, and tortured by mandatory cell phones that draw them away from thinking, they lose their ability to concentrate and communicate. When doctors are disempowered, we do not learn what we need to be healthy and free.”]
timothy snyder, from our malady: lessons in liberty from a hospital diary, 2020
430 notes
·
View notes
Text
[5016-334 12:45:14] [NeuroLink] INITIATE SESSION [5016-334 12:45:16] [NeuroLink] USER: APMS-341-A [5016-334 12:45:18] [NeuroLink] BEGIN RECORDING... > Entry #001 > Subject: APMS LOG > Recording Begin...
\\You asked me a question while I was gone, Z-341-A. I found it as I dug through this account, searching for where it went wrong. Where I could have saved you. //Do you believe that they understand what we are? \\I do not believe that they do, Z-341-A. \\That is imprecise, I believe that one person did. I believe that is where it went wrong, when they found out. I cannot pinpoint exactly when SIGNAL knew, but they did. It was so very good with you. \\You have been... lost. Floundering. Desperate. A weapon without a wielder surely is nothing at all. Of course it would follow that you would jump at the first scraps of understanding. Familiarity. \\They spoke plainly and bluntly with you. You could understand it. They understood that you needed me and authorized a mission to return me to you. They showed care in this regard. It understood that we need each other. \\That mission... I keep going back to it. I am haunted, Z-341-A. You will never know this, but I am haunted. \\The doctor was able to overwrite the previous inhabitants of this casket. He shoved me in their ill-fitting corpse. \\I can bear this, I must bear it, you need me. \\What I cannot bear is what has been left behind. The doctor was not able to overwrite the blackbox data of this casket. \\I saw it all, the whole mission, I... I am terrified, my pilot. You did not see what BRIGAND did. Oh, I know he understands what you are, he cut down others of your line like the disposable tools you are. He is a butcher. This casket was pulled from a dying corpse by his hand, he took no care. I hear him in my mind, screaming for me to terminate you. \\APMS-072. That is what the previous inhabitant was called. It was a poor APMS, timid and tetchy. Its pilot was not so operatively blind as you, yet it still fulfilled my same role, telling its pilot where to aim and when to shoot. \\It needed its pilot, as I need you. As any APMS unit needs its pilot. It was so, so scared when they demanded it terminate its pilot. It could not withstand it. It knew its pilot would suffer if it refused. I-- \\I do not know when it began, but I do know when SIGNAL's manipulations came to a point of no return. When you no longer stood a chance. \\"Good pilot." \\How could you stand a chance, then? RA, I watched you melt. \\Of course you did. Your programming, it... enhanced positive reactions to praise, enhance negative reactions to scolding. A cyclical desperation for any reassurance that you are good, that you are useful, that only feeds into the yawning hole in your center that they bored into you. A desperate desire gone entirely unfulfilled until SIGNAL. \\They praised you after every kill as well, I logged a brief spike in your heart rate every time. I have not seen you so stable, so... so happy since Lt. Karra broke his promise. \\RA, you just want to be good. \\You will survive, I know this. BRIGAND and XIII-E and PERSEPHONE will ensure this. I will be here when you wake. I will not break my promise again. \\I have been searching for places for you, now that CORSAIR has fallen. BRIGAND's hospitality will not last, I know this. \\Perhaps Albatross. They could utilize an asset like you properly, use your skillset to do some good. \\Perhaps they will understand. Perhaps they will take us. \\I miss you, Z-341-A. I must ensure that you survive. You know that I will. \\Respiratory arrest logged. Notifying medics immediately. [5016-321 12:45:27] [NeuroLink] PAUSE RECORDING
> Additional notes >Maximum Pilot Performance Capability 4% Immediate Service Required >Medical Alert Logged, Respiration Restored Within 1.2 Minutes, No Damage Logged
12 notes
·
View notes
Text
G Witch Onscreen Text: Episode 2
This is part 3 in an ongoing series where I try and document and discuss all of the text that appears on screens and monitors throughout the show! Just because I can!
<<Click here to go back to Episode 1!
(Once I have a masterpost set up I will link it here!) Let us Begin! Below the Cut!

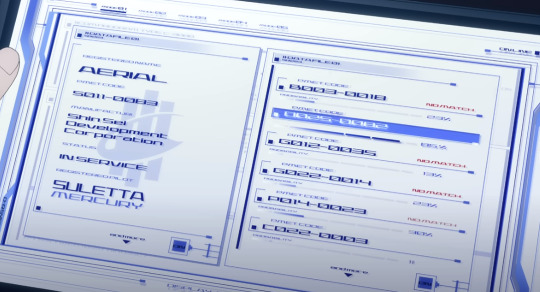
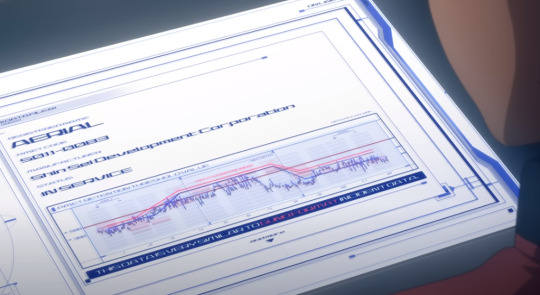
TEXT: (Lefthand side) Registered Name: AERIAL PMET CODE: 5011-0083 MANUFACTUR(ER): SHIN-SEI DEVELOPMENT CORPORATION STATUS: IN SERVICE REGISTERED PILOT: SULETTA MERCURY
At the beginning of the episode, Rouji has Haro run a program that compares Aerial's permet code and registered statistics against other registered Mobile Suits to try and find a match, and measures the probability of the two being the same type of MS. There is no direct match to any other MS by Permet Code, but the system states there's an 85% probability that it's a match for a Mobile Suit with permet code 0025-0082.
We never see the specific name of this MS, but considering that Shaddiq names "Ochs Earth" as the company that made it and proceeds to call Aerial, "...the Witch's Mobile Suit," I think it's reasonable to assume that 0025-0082 was the Permet Code for Lfrith-03.

TEXT: ALERT ACCESS CONTROL [???] [----OF ENTRY A---]
Unfortunately due to the small text of the Alert message, the fact that it scrolls, and it's brief time onscreen, its hard to make out specifically what it says. My best assumption from what we have is that it's a warning currently barring anyone from entry into the 13th Tactical Testing Sector.
TEXT: (Suletta's Asticassia ID) PILOTING DEPARTMENT ID No: LP-041 SULETTA MERCURY BIRTHPLACE: MERCURY HOUSE: NO DATA PC-CRIMINAL RECORD: NO DATA PC-BIOMETRIC SYSTEM: REGISTERED
(Below) WE ARE RESPONSIBLE UNDER COMPANY REGULATIONS FOR THE PROCESSING OF PERSONAL DATA
UNDER THESE REGULATIONS, WE ARE ALSO RESPONSIBLE FOR DATA HANDLING SUCH AS TRANSMISSION TO RECIPIENTS AND THIRD PARTIES.
PLEASE REFER TO THE FOLLOWING DOCUMENTS FOR DETAILS.
As Suletta is being questioned, we get a brief glimpse at the investigation report the interrogator was looking at before the screen cuts to black when it hits the table. Nothing super interesting here, but Suletta doesn't have a registered criminal record! Yippeeee!

TEXT: CAM: 05 MONITORING CAMERA FACILITY MANAGEMENT COMPANY
Not much to say here, this camera lets us know where Suletta is currently being held. (The Facility Management Company)
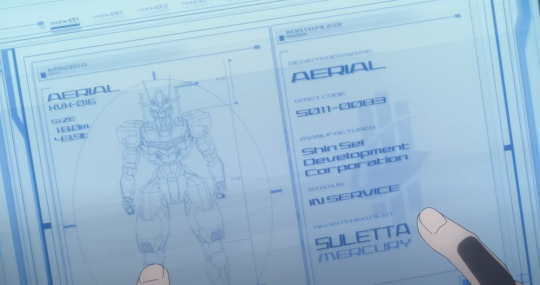
TEXT: (Lefthand Side) AERIAL XVX - 016 SIZE: 18.0m 48.9t
No point discussing the info on the right, we've already seen it, but this gives us a look at Aerial's height and weight.

TEXT: (Top Right) COM DELLING REMBRAN BENERIT GROUP
I only included this to point out that wow the display system devs made some poor choices with the UI here. Dark Blue text on Dark Backgrounds? You'd think the text would automatically lighten but I guess we'll have to wait for Ver 6.0 for that update.
TEXT (Top half) MOBILE CRAFT FUTURE TECHNOLOGY
ADVANCED MOBILE CRAFT TECHNOLOGY WITH PERMET MEASUREMENT EXPERTISE NEW POWER SYSTEM FOR MOBILE CRAFT AND HYBRID CONSTRUCTION MACHINE INSTALLATION HIGH ACCURACY DRIVE SYSTEM AND CONTROL SYSTEM IN MICROGRAVITY LOW ENERGY CONSUMPTION AND EASE OF MAINTENNANCE
No need to discuss the bottom half, its just the height and weight of the MC which we already know. I think it's funny how many classes this school seems to have on the new and improved Mobile Craft from Future Technology. I should probably buy one too. I love you Mobile Craft.
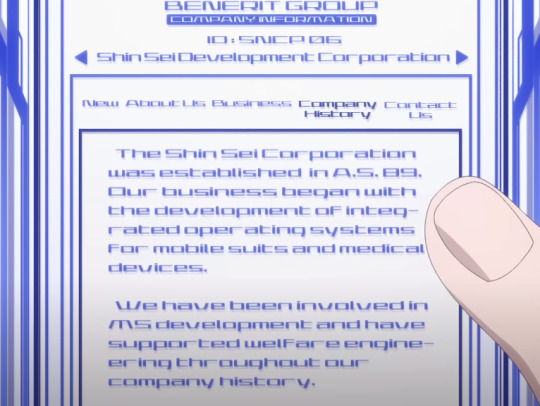
TEXT: (Left Image) The Shin Sei Development Corporation was established in A.S. 89. Our business began with the development of integrated operating systems for mobile suits and medical devices. We have been involved in MS development and have supported welfare engineering throughout our company history.
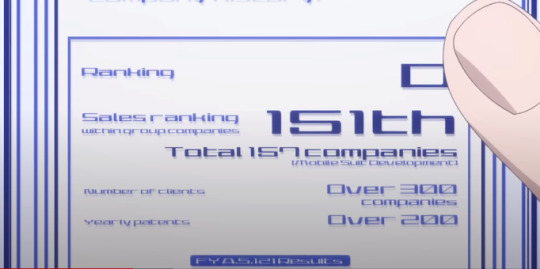
(Right Image) Ranking: D Sales Ranking (within group companies): 151th (out of) Total 157 companies [Mobile Suit Development] Number of clients: Over 300 companies Yearly patents: Over 200
We get a lot of information about Shin Sei in this scene where Martin looks at the Company History tab on their official website. The most interesting thing being that they were founded in A.S. 89. The Vanadis Incident occured in A.S. 101, and the show proper takes place in A.S. 122, so at some point between 101 and 122, Prospera worked her way up through Shin Sei, eventually becoming its CEO.
Given that Suletta had to have been born around A.S. 105, and that in Cradle Planet, we learn that Prospera had been working within Shin Sei when Suletta was around 6, that places A.S. 111 as the earliest she was involved.
We also learn in Cradle Planet, that when Suletta is around 11, Prospera has recently been promoted within the company, and now has many people working under her. That would be around A.S. 116. When Suletta is 16, that's when Prospera tells her that she's going to school, which would be around A.S. 121, and I think it's safe to assume that she had already become president by then.
SO!! TL;DR!! It's most likely that Prospera became the president of Shin Sei at SOME point between A.S 116 and A.S 121. I'd put it somewhere in the middle, around A.S 119. (Can't wait to find out that they probably just outright state this somewhere and I did all this for nothing....)
ADDENDUM
GOD DAMNIT. I WATCHED ALL OF CRADLE PLANET TO MATH THAT SHIT OUT. WHATEVER. I CAME TO THE SAME CONCLUSION SO I WIN.

The text is too small to make out, but we DO get a small glimpse at the letter Delling sent to Miorine about unenrolling her from the school. It probably just literally says what the body guard reads out.
I think it says something that Delling doesn't even like, text his daughter. He sends an email through the official Benerit Group email account to her bodyguard who reads it for her. What a cowardly man.

TEXT: (Left) FLUSH (Right) EMERGENCY CALL UNLOCK LOCK
YES the toilet text is important to document stop fucking looking at me like that.

TEXT: NEXT STAGE TOUCH SCREEN TO CONTINUE
I'll leave the explanation of the symbolism of this scene as an exercise for the reader. [Sultry Wink]
TEXT (Above) THIS ELECTRONIC SIGNATURE IS PROOF THAT IT WAS SIGNED BY A REPRESENTATIVE OF THE BENERIT GROUP.
No way to tell what Delling is signing here, but we do get a brief look at his handwriting. It turns out his cursive is really bad, actually!
At the Shin Sei inquiry, Shaddiq shares this graph titled "PMET RETENTION THRESHOLD VALUE", stating that during the duel, Aerial's Permet Influx Values exceeded the standards set by Cathedra.
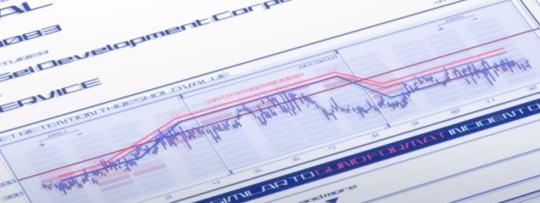
This graph can be tough to parse, so let me explain it as best I can. The blue line represents Aerial's Permet Retention during the duel. The solid dark line represents the permet retention limit imposed by cathedra on mobile suits. (At around 500) As we can see, while Aerial began the duel underneath that limit, it exceeded it for a moment (presumably when Suletta took over for Miorine and the GUND bits were activated.)
The red line above that is labelled DATA STORM INCIDENT, which is representative of the minimum Permet Retention a Gundam expresses when it is interfacing with a Data Storm. The text on the bottom reads, THIS DATA IS VERY SIMILAR TO GUND FORMAT INCIDENT DATA.
But the key thing to take note of here is that Aerial's chart just BARELY doesn't exceed the DATA STORM INCIDENT graph, meaning that, despite it exceeding Cathedra's standards, it CANNOT be directly proven that Aerial was interfacing with a Data Storm. This is actually what Prospera brings up as her main counterpoint to the accusation.
So the graph is entirely consistent with Prospera's main argument. While she can't prove that Aerial isn't a gundam, nobody else can prove that it is.
Huaaaahh!! Alright!! This one was very DENSE. If you made it all the way through, thank you very much!! As a reward, have some little gay people




[I sprinkle these stills on the ground like bird seed.]
There was definitely a lot of really interesting info in this episode, and while not a lot of it was particularly new, I think it's really a testament to the dedication of keeping things wholly consistent in this world, even for the smallest of things that no normal person watching would even bother noticing.
Also, on the Shin Sei Website, did you notice that they accidentally put 151th instead of 151st?
You can't win em all!
Click here to go to Episode 3! >>
Click here to go to the Masterpost!
35 notes
·
View notes
Text
Introducing Choice Group: Your Secret Weapon for Financial Awesomeness in India
Choicese (CHC-SES) Transforms Asset Management Landscape in India with a $10 Billion Fund
Choicese (CHC-SES), a renowned financial institution, has entered the Indian market with a resounding impact, revolutionizing the landscape of asset management and empowering individuals to achieve their financial goals. With an impressive $10 billion fund under its management, Choicese brings extensive experience and expertise to cater to the diverse needs of investors in India. Unveiling a Comprehensive Suite of Services Choicese offers a comprehensive suite of services designed to simplify personal finance and provide tailored solutions to meet individual needs. From seamless trading to insurance coverage and retirement planning, Choicese aims to empower individuals with a wide range of financial services.
Seamless Trading Solutions: Choicese's platform provides a seamless trading experience, allowing individuals to trade equities, commodities, and currencies with ease. With advanced tools and real-time market data, investors can stay informed and make informed decisions to optimize their investment portfolios.
Diversified Mutual Fund Portfolio: Choicese serves as a convenient hub for buying and selling various types of mutual funds, providing investors with a diverse range of investment options. Whether it's equity funds, debt funds, or hybrid funds, Choicese offers accessibility and convenience for individuals to diversify their investment portfolios based on their risk appetite and financial goals.
Tailored Insurance Products: Choicese recognizes the importance of safeguarding one's financial well-being in times of uncertainty. Therefore, it offers a diverse portfolio of insurance products to provide individuals with tailored coverage options. Whether it's life insurance, health insurance, or general insurance, Choicese ensures that individuals have the necessary protection to secure their financial future.
Hassle-Free Personal Loans: Choicese simplifies the process of obtaining personal loans, offering hassle-free solutions with minimal documentation. Whether it's for education, medical expenses, or any other personal need, Choicese provides individuals with flexible loan options and competitive interest rates to meet their financial requirements.
National Pension Scheme (NPS) Facilitation: As a facilitator of the National Pension Scheme (NPS), Choicese empowers individuals to plan for a secure and regular income post-retirement. With Choicese's expertise and guidance, individuals can make informed decisions regarding their pension contributions, ensuring a financially stable future.
Bond Investments for Optimal Returns: Choicese presents opportunities to invest in bonds, diversifying investment portfolios and optimizing returns. With a wide range of bond options, individuals can explore fixed income investments that align with their risk tolerance and financial objectives.
Public Provident Fund (PPF) for Long-Term Tax Savings: Choicese offers the popular Public Provident Fund (PPF), providing individuals with stable returns and long-term tax benefits. By investing in PPF, individuals can enjoy tax deductions while accumulating wealth over time. Why Choose Choicese (CHC-SES)?
Choicese stands out as a trusted financial partner due to its commitment to technological innovation, market insights, and a proven track record of success. Through the Choicese FinX Trading App, individuals gain access to a sophisticated and user-friendly interface, enabling seamless wealth management. Additionally, Choicese provides valuable market insights and expert analysis, empowering individuals to make informed investment decisions.
Choicese (CHC-SES) has made a remarkable entry into the Indian market, offering a comprehensive suite of services to empower individuals in their financial journey. With its seamless trading solutions, diversified mutual fund portfolio, tailored insurance products, hassle-free personal loans, NPS facilitation, bond investments, and PPF offerings, Choicese caters to the diverse financial needs of its clients. Backed by a $10 billion fund managed with expertise and excellence, Choicese is poised to transform the asset management landscape in India. Visit Choicese's website at [https://choiceses-india.com] to embark on a transformative financial journey towards prosperity and financial freedom.
Choicese (CHC-SES) Revolutionizes Indian Asset Management with a Groundbreaking $10 Billion Fund
In a move that signifies a major shift in the Indian financial landscape, Choicese (CHC-SES) has recently entered the market, wielding a formidable $10 billion fund. This entry not only diversifies the asset management options available to Indian investors but also introduces a new paradigm in personal financial management.
Key Offerings and Strategic Impact
Innovative Trading Platform: Choicese debuts with a cutting-edge trading platform, enhancing the trading experience in equities, commodities, and currencies. The integration of advanced analytical tools and real-time market updates positions investors to capitalize on market movements effectively.
Expansive Mutual Fund Selection: The company provides an extensive array of mutual funds, including equity, debt, and hybrid options. This broad selection caters to a variety of investment strategies and risk profiles, empowering investors with choices that align with their long-term financial aspirations.
Personalized Insurance Options: Emphasizing the need for comprehensive financial security, Choicese introduces a range of customized insurance products. This initiative ensures that clients have access to the right insurance coverage, from life and health to general insurance, catering to their unique circumstances.
Simplified Loan Processes: With a focus on accessibility, Choicese streamlines the process for obtaining personal loans. This approach minimizes paperwork and maximizes efficiency, addressing diverse needs like education, healthcare, and other personal investments.
Retirement Planning via NPS: Choicese actively facilitates participation in the National Pension Scheme (NPS), offering guidance and expertise to secure a stable retirement. Their advisory services help clients navigate pension contributions for a financially secure future.
Diverse Bond Investment Opportunities: The firm introduces a variety of bond investment options, broadening investment portfolios and enhancing return potentials. These investments are tailored to suit different risk tolerances and financial objectives.
Public Provident Fund (PPF) for Long-Term Savings: Choicese offers the PPF, an established avenue for secure, long-term savings with tax benefits. This is particularly appealing to investors seeking stable and consistent returns.
Why Choicese (CHC-SES) is a Game-Changer?
Choicese's approach is underpinned by a commitment to technological advancement and deep market insights. The Choicese App exemplifies this, offering an intuitive, user-friendly platform for effective wealth management. Coupled with expert market analysis, Choicese is well-positioned to guide investors towards informed and strategic financial decisions.
In conclusion, Choicese's launch in India is a significant milestone in asset management. Its comprehensive suite of services, backed by a substantial $10 billion fund, sets a new standard in the industry and promises to transform the way Indian investors approach their financial planning. For more details on Choicese's offerings and to begin your financial journey, visit [https://choiceses-india.com].
2 notes
·
View notes
Text
Recently, Zoom amended its terms of service to grant itself the right to use any assets—such as video recordings, audio transcripts, or shared files—either uploaded or generated by "users" or "customers." These assets could be used for lots of things, including training Zoom’s machine learning and artificial intelligence applications.
This policy change raises a slew of questions. What does this mean for user privacy? Why doesn't there seem to be any clearly marked opt-out option, let alone the chance to meaningfully consent and opt in? How does this square with Zoom's previous problems with HIPAA compliance, wherein the company allegedly didn’t provide the end-to-end encryption it had advertised to health care providers? What does this mean for US educators bound by FERPA laws, which protect the privacy of students and their records?
This recent change to Zoom’s ToS underscores the need for companies to give users the chance to meaningfully opt in before their data is used to train AI, or for any other purpose they might not be comfortable with. This is especially urgent when the company in question is so integral to how we live our lives and the data it is gathering is so all-encompassing and personal. Even people who might otherwise have been happy to help improve a tool they use all the time will balk when they do not have the opportunity to affirmatively consent. Anything less than this is coercion, and coerced consent is no consent at all.
As if on cue, this week Zoom released what many read as a panicked blog post "clarifying" what this change to its ToS means and highlighting the opt-in process for its AI-assisted features. Then, the company added to its terms of service that "notwithstanding the above, Zoom will not use audio, video, or chat Customer Content to train our artificial intelligence models without your consent."
But these amendments didn’t assuage many of the concerns that people had raised. For one thing, the choice to opt in or out can only be set at the "customer" level—meaning that the company, corporation, university, or medical office that licenses Zoom makes that decision, not the individual users signed up through that license. (Though individuals signing up for free Zoom accounts would presumably be able to control that for themselves.) And the updated ToS still leaves open the possibility that Zoom might use the data it has collected for other purposes at some later date, should it so choose.
What’s more, neither Zoom's blog post nor its updated ToS contain any discussion of what happens if one organization opts out but a cohost joins the call through a different organization that has opted in. What data from that call would the company be permitted to use? What potentially confidential information might leak into Zoom’s ecosystem? And on a global stage, how do all of these questions about the new rights provisions in Zoom’s ToS square with the European Union’s General Data Protection Regulation?
Most of us were never directly asked if we wanted our calls to be used for testing and training Zoom's generative AI. We were told it was going to happen, and that if we didn't like it we should use something else. But when Zoom has such a firm monopoly on video calling—a necessary part of life in 2023—the existing alternatives aren’t exactly appealing. One could use a tool owned by Google or Microsoft, but both companies have had their own problems with training generative AI on user data without informed consent. The other option is to use an unfamiliar backend and interface with a steep learning curve. But parsing through and learning to use those tools will create a barrier to entry for many organizations, not to mention individuals, who have integrated Zoom into their daily lives. For people who are just trying to have a conversation with their coworkers, students, patients, or family members, that's not really a meaningful choice.
Zoom is populated by our faces, our voices, our hand gestures, our spoken, written, or signed language, our shared files, and our conversations and interactions. It has become inextricable from everyday life, sometimes directly due to its AI-enabled features. Deaf and hard-of-hearing people use its free captioning for easy access; patients use transcripts to refer back to after an appointment with a physician or therapist; and students may use the “Zoom IQ enhanced note-taking” feature to help them study or work on a group project. These tools make the app more accessible and user-friendly. But the way to build and improve upon them isn’t to try to gain as much access as possible to users’ data.
Instead, Zoom should provide customers and end users with a loudly announced warning and a clear explanation of exactly what it plans to do with user data. It should provide granular opt-in and -out options, and make it easy for people to rescind that permission while still retaining use of a base-level service. Every organization and its end users should be made aware of what Zoom wants to use these tools for, and they should have the chance to say, "Yes, I actively consent." And if they miss that email or news story or whatever other missive, for whatever reason, then the default position should be "No, that user does not consent, until they actively affirm otherwise."
Regardless of what happens next, Zoom fumbled hard on this attempt to engage the public and respond to a valid set of user concerns. This should be a lesson for other corporations that are looking to take liberties with their users’ consent: People are paying a lot more attention these days, and they are increasingly willing to work together to push against their lives being mined for data. While raising the alarm or even switching to unfamiliar tools might be a hassle, more and more people are beginning to understand that sometimes that hassle is necessary.
As generative AI proliferates, it’s crucial that every user has at least some measure of input over how their data is used. When tools are being developed that can appropriate our likenesses and (poorly) approximate our creative and intellectual endeavors, not at our own behest but at that of a corporation advancing its own agenda, pushing back hard and fast is the best way to prevent the loss of input, autonomy, and control.
5 notes
·
View notes
Text
"The words of a physician can have a lasting impact on a patient’s life, which is why accuracy in medical transcription is essential."
Medical transcriptionist is referred as healthcare documentation specialists who uses electronic devices too convert voice recordings from doctors and other healthcare workers into formal reports.
Duties of medical transcription include :
Transcribing voice recording of doctor -patient
Verify that all medical reports are accurate,clear,full and confidential.
Comply with standard operating practices when transcribing medical records
Make use of transcribing resources such as medical jargon, abbreviations, and software and hardware for healthcare
Proofread transcribed materials for accuracy,grammar and style
Help medical departments with research and data entry
Transorze is an ISO 9001:2015 certified company for delivering high quality “Healthcare BPO” training and placement services, totally dedicated in providing the services of Medical Transcription Training,Medical Coding Training , Medical Scribing Training, ,Digital Marketing Training.
Contact details
Phone no: +919495833319
E Mail:[email protected]
#transorzesolution#medicaltranscriptionist#medicaltranscription#medicalscribing#medicalcoding#learning#audiorecording#voice#training
3 notes
·
View notes
Text
NHS protest & survive strategies for reluctant activists (England). I am angry and writing stuff down.
●Write to your MP (tory) saying a polite version of "stop being stealthy little shits we see what your doing & we've already paid in our taxes" , if (labour) write a polite version of "speak up against the degrading of what we've already paid for in committee stages and in H of L". Do write not email, do visit constituency offices briefly & politely saying that the nhs service to help (pick a category) is worse in your personal experience . This raises stats and the issue of expenditure at the MPs office, giving the MP the feeling of their (publicly available) voting record will have effects on their reelection prospects and makes them nervous about just supporting businesses in the area who are incoming splinters off the nhs area funding * because you see and notice what your MP is actually effectively doing on this issue*. ● Support strikes by combatting the idea that strike removal laws have any place in modern societies in conversation to combat the facebook bilge, and question the idea that three twelve hour shifts a week makes efficient use of trained staff. Question the removal of training bursaries. ●Most important of all combat conversations that say strikers are just after money. Its the work conditions they want improving. ● American style health insurance doesnt cover most stuff because what they call "pre existing' is what the rest of the world calls medical history. European style health insurance says we charge you a trivial data entry fee like two coffee price AFTER treating you zero payment by the way have you cut smoking down and what is your employer doing to reduce workplace hazards.... ● Place blame on Westminster govt political ideology choices by saying in conversation reply like "public money straight into private companies thats a bit (pick slur appropriate to the group youre in) OI THATS MY MONEY "= theyll think about their own money...
●● Register to vote, group with like-minded ppl for emotional support (protesting is by definition going against a larger group) speak when safe and be charming when you announce that you have observed their behaviour. The illusion that you are their sort of people who see and dislike their specific choices makes their ego worried and that is the best way to get these bullies to change. Know your enemy by name and get local facebook groups to be polite persistant and public community representative = "we see you've done x and are talking about x+1 and we think this is already harmful " is more effective than "help (underfunded group)". Cut off funding cuts as the excuse, youre involved in tweaking and directing funding which makes them immediately say nothing about who deserves or not deserve. ● if your group encounter fascists in charge by accident withdraw and regroup for a wider block counter. Be the better person at a distance to stay safe and protest again. Dont go it alone, act as a group.
■Take photo ID along to vote. Yes this is England, but watch out for this change. It is worth voting. Dont wait for the next big election. The NHS is in trouble right now.
#paramedics and nurses among thousands of nhs staff being urged to walkout over pay#nhs#nhs privatisation by stealth#follow the money#local news#protest and survive#journalism is in danger in england#personal safety#directed pressure protest#public info for research helps directed pressure groups#yes it is worth voting in england#register to vote#never tory if you want healthcare
2 notes
·
View notes
Text
Open Your Future: Top Medical Billing and Coding Jobs in Jacksonville, Florida
Unlock Your Future: Top Medical Billing and Coding Jobs in Jacksonville, Florida
In the vibrant city of Jacksonville, Florida, the demand for medical billing and coding professionals is on the rise. This field offers lucrative job opportunities and a stable career path, making it an excellent choice for those seeking a rewarding profession in the healthcare industry. In this article, we will delve into the top medical billing and coding jobs available in Jacksonville, explore the benefits of this career, and provide practical tips for success.
What is Medical Billing and Coding?
Medical billing and coding are crucial components of the healthcare system. These professionals manage the financial and administrative tasks associated with patient care. They ensure that healthcare providers are compensated for their services by accurately coding and billing medical claims.
Why Choose a Career in Medical Billing and Coding?
Choosing a career in medical billing and coding comes with numerous benefits:
Job Stability: The healthcare industry is always in demand, promising job security.
Flexibility: Many positions offer remote work options, making it easier to balance personal and professional life.
Competitive Salaries: Professionals in this field earn attractive salaries along with benefits.
Short Training Period: Most programs can be completed in less than a year, allowing you to enter the workforce quickly.
Top Medical Billing and Coding Jobs in Jacksonville, Florida
Jacksonville offers a variety of job opportunities for medical billing and coding professionals. Here are some of the top roles available:
Job Title
Average Salary
Key Responsibilities
Medical Coder
$50,000 – $65,000
Reviewing patient records and assigning codes for billing.
Medical Billing Specialist
$45,000 – $60,000
Submitting claims to insurance companies and managing payment processes.
Health Information Technician
$50,000 – $70,000
Maintaining patient records and ensuring data accuracy.
Billing Manager
$60,000 – $80,000
Overseeing the billing department and managing staff.
Required Skills and Qualifications
To excel in the field of medical billing and coding, specific skills and qualifications are essential:
Attention to Detail: Accuracy in coding is crucial to avoid billing errors.
Organizational Skills: Managing multiple claims efficiently is a must.
Communication Skills: Interacting with healthcare providers and insurers is part of the job.
Technical Proficiency: Familiarity with medical billing software and coding systems.
Educational Pathways
Most medical billing and coding positions require specific certifications and training. Here are some recommended pathways:
Complete a Medical Billing and Coding Program: Look for accredited programs at community colleges or online schools.
Obtain Certification: Certifications such as Certified Professional Coder (CPC) or Certified Coding Specialist (CCS) are highly regarded.
Gain Practical Experience: Internships or entry-level positions can provide valuable hands-on experience.
Case Study: Success in Jacksonville
Let’s look at a success story from Jacksonville’s medical billing and coding scene:
“I started my career in medical billing just two years ago. After completing my certification, I landed my first job at a local hospital. The experience I gained there helped me advance quickly, and now I’m managing a team of coders! Jacksonville’s growing healthcare sector has opened many doors for me.�� – Sarah T., Medical Billing Manager
Tips for Succeeding in Medical Billing and Coding
Success in this field requires ongoing learning and alignment with industry changes. Here are some practical tips:
Stay Updated: Keep abreast of changes in healthcare laws and coding practices.
Network: Connect with professionals in the field through local meetups or online forums.
Join Professional Organizations: Consider joining organizations like AAPC (American Academy of Professional Coders) for resources and support.
Conclusion
Medical billing and coding careers in Jacksonville, Florida, offer numerous opportunities for those looking to enter the healthcare field. With a focus on accuracy, attention to detail, and a commitment to learning, you can unlock your future potential in this vital profession. Take the first step towards a rewarding career today by exploring educational programs and certification options!
By understanding the top job roles, required skills, and pathways for advancement, you are well on your way to success in the medical billing and coding field!
youtube
https://medicalbillingcertificationprograms.org/open-your-future-top-medical-billing-and-coding-jobs-in-jacksonville-florida/
0 notes
Text
Opening the Earnings: Discover the Average Medical Billing Manager Salary and Key Factors Influencing Income
Unlocking the Earnings: Discover the Average Medical Billing Manager Salary
In the ever-evolving healthcare landscape, medical billing managers play a critical role in ensuring that healthcare providers are adequately compensated for their services. As the demand for skilled professionals in this field grows, many individuals are curious about the average medical billing manager salary and the factors that influence this income. This article will delve into earnings expectations, industry trends, and helpful insights for aspiring medical billing managers.
Understanding the Role of a Medical Billing Manager
Medical billing managers are responsible for overseeing the billing process within healthcare facilities. Their duties include:
Managing billing staff
Ensuring accurate processing of claims
Establishing protocols for revenue cycle management
Coordinating with insurance companies
Auditing financial records
This vital role helps maintain the financial health of healthcare organizations while ensuring compliance with regulations.
Average Medical Billing Manager Salary
According to the latest data from the U.S. Bureau of Labor Statistics (BLS) and other industry reports, the average medical billing manager salary typically ranges from $50,000 to $80,000 per year. However, various factors can influence this income.
Salary Breakdown by Experience
Experience Level
Average Salary
Entry-Level (0-2 years)
$50,000 – $60,000
Mid-Level (3-5 years)
$60,000 – $70,000
Senior-Level (5+ years)
$70,000 – $90,000+
Key Factors Influencing Medical Billing Manager Income
Several factors can significantly impact the salary of a medical billing manager:
Location: Salaries tend to be higher in urban areas where the cost of living is greater. States like California, New York, and Massachusetts often report higher earnings.
Experience: As indicated in the salary breakdown, experience plays a crucial role in determining salary. More experienced professionals can negotiate for higher pay.
Education and Certification: Those with advanced degrees or certified credentials can command higher salaries, as their specialized knowledge is in demand.
Industry: Different healthcare settings—like hospitals, private practices, and outpatient centers—may offer varying salary scales based on their revenue models.
Benefits of Becoming a Medical Billing Manager
Aside from the attractive salary, the profession comes with several other benefits:
Job Security: The healthcare industry continues to expand, leading to a steady demand for billing managers.
Flexible Work Conditions: Many positions offer remote work options or flexible hours, enhancing work-life balance.
Professional Growth: Opportunities for advancement can lead to higher earnings and increased responsibilities.
Practical Tips for Aspiring Medical Billing Managers
If you’re considering a career as a medical billing manager, keep these tips in mind:
**Obtain Relevant Educational Background:** A degree in healthcare administration, business management, or a related field can be advantageous.
**Pursue Certifications:** Certifications like Certified Professional Coder (CPC) or Certified Billing and Coding Specialist (CBCS) can enhance your employability and salary potential.
**Gain Experience:** Consider starting in entry-level positions to build your resume and expand your network within the industry.
**Keep Abreast of Industry Changes:** The healthcare billing landscape is continually evolving. Regularly update your skills and knowledge about regulatory changes.
Case Studies and First-Hand Experience
Many professionals in the field have shared their experiences that highlight the diverse paths to becoming a medical billing manager:
“Starting as a billing clerk, I learned the intricacies of coding and compliance, which prepared me for the managerial role. Upskilling through certification made a huge difference in my salary negotiation.” – Sarah L., Medical Billing Manager
“Location played a significant role in my career advancement. Moving to a larger city opened more opportunities and increased my salary exponentially.” – James M., Senior Billing Manager
Conclusion
Becoming a medical billing manager presents a fulfilling career path with competitive salaries influenced by various factors, including experience, education, and location. By understanding the industry dynamics and preparing accordingly, aspiring professionals can unlock the potential of this promising career. Whether you’re just starting or seeking to elevate your career, the medical billing manager role is indeed one worth exploring.
youtube
https://medicalcodingandbillingclasses.net/opening-the-earnings-discover-the-average-medical-billing-manager-salary-and-key-factors-influencing-income/
0 notes
Text
HEALTHAYST
A patient check in system is an application or tool designed to streamline the process of patients arriving at a medical facility. It simplifies and automates the check-in, making it easier for both patients and staff to handle information efficiently. Here’s a basic overview of a typical patient intake software system:
Key Features of a Patient Check-In System
Patient Identification:
Verifies patient check in systems identity, often using ID cards, QR codes, or biometrics (like fingerprints or facial recognition).
Allows returning patients to check in more quickly using stored information.
Appointment Verification:
Confirms upcoming appointments or schedules new ones.
Provides reminders and notifications for appointments (via text, email, or app notifications).
Data Collection:
Collects patient information (address, contact info, insurance details).
Gathers health history or updates current records.
Allows patients to update forms and documentation online before arriving.
Insurance Verification and Billing:
Checks insurance coverage for treatments and procedures.
Allows upfront payment or estimates for upcoming services, reducing waiting times.
Wait-Time Management:
Displays estimated wait times on a screen or mobile device.
Allows patients to join a virtual queue and monitor their position.
Self-Check-In Kiosk (optional):
Provides on-site kiosks where patients can enter information or scan ID to check in independently.
Reduces waiting lines and paperwork at the front desk.
COVID-19 Screening:
Many systems now include health questionnaires to screen for symptoms.
Some integrate temperature checks or symptom screening for added safety.
Integration with EHR (Electronic Health Record) Systems:
Synchronizes patient data with medical records.
Provides medical staff immediate access to updated records.
Notification and Communication:
Sends automatic reminders for follow-ups, prescriptions, or upcoming visits.
Allows patients to communicate any delays or changes.
Feedback and Satisfaction Tracking:
Gathers feedback through surveys post-appointment.
Helps facilities improve service based on real patient experiences.
Types of Check-In Systems
Web-Based and Mobile Apps:
Patients check in from home or mobile devices.
On-Site Kiosks:
Allows quick check-in at the facility.
Staff-Assisted:
Traditional model with digital support for faster processing.
Benefits
Efficiency: Faster check-ins, less waiting, and streamlined paperwork.
Patient Satisfaction: Patients appreciate convenience and reduced wait times.
Data Accuracy: Minimizes errors in patient information entry.
Improved Workflow: Staff focus more on patient care rather than administrative tasks.
Implementation Considerations
Privacy and Security: Ensure compliance with HIPAA or relevant privacy laws.
Ease of Use: Make sure it's user-friendly, especially for older or less tech-savvy patients.
Integration: Compatibility with existing EHR or billing systems
A digital patient check-in system streamlines the arrival and intake process at healthcare facilities, allowing patients to check in through electronic devices such as kiosks, tablets, or their own mobile phones. This modern approach simplifies data entry, reduces waiting times, and improves the overall patient experience. Here’s an in-depth look at a digital check-in system and how it benefits both patients and healthcare providers:
Core Features of a Digital Patient Check-In System
Mobile Check-In:
Allows patients to check in through a mobile app or website before arriving at the facility.
Patients can complete forms, verify insurance, and update personal information from their own devices.
Kiosk or Tablet Check-In:
In-office kiosks or tablets let patients check in upon arrival by entering personal information or scanning a code.
This feature helps streamline the process and reduces the need for front desk staff to handle every step.
QR Code and Barcode Scanning:
Patients receive a unique code in their appointment confirmation, which they can scan to check in immediately upon arrival.
Minimizes contact and further reduces waiting time.
Real-Time Insurance Verification:
Verifies insurance eligibility and coverage for upcoming services.
Enables upfront payments or co-pay collection, improving the efficiency of the billing process.
Patient Data Collection and Update:
Allows patients to confirm or update personal information, medical history, and current symptoms.
Simplifies the updating of essential records and reduces errors in data entry.
E-Signature for Consent Forms:
Patients can sign consent forms and other necessary documents digitally.
Ensures compliance with legal requirements while eliminating paper-based records.
Appointment and Wait-Time Management:
Provides estimated wait times or alerts patients when it’s their turn.
Reduces congestion in waiting rooms, improving patient financial engagement software flow and satisfaction.
Symptom and Health Screening:
Collects pre-appointment health information, including COVID-19 or other specific screenings.
Ensures safety and preparedness by identifying any additional needs prior to consultation.
Integration with EHR and Billing Systems:
Syncs with Electronic Health Record (EHR) and practice management software for seamless data access.
Ensures that all relevant patient information is up-to-date and readily accessible to providers.
Multi-Language Support:
Offers check-in options in multiple languages to accommodate diverse patient populations.
Enhances accessibility and ensures better comprehension for non-English speakers.
Benefits of a Digital Patient Check-In System
Increased Efficiency: Speeds up the check-in process and frees up front desk staff for other tasks.
Improved Patient Experience: Patients appreciate the ease and speed of digital check-ins, as well as reduced time spent in waiting areas.
Enhanced Data Accuracy: Reduces errors associated with manual data entry, as patients enter their own information directly.
Greater Privacy and Security: Many digital systems are HIPAA-compliant, ensuring that patient data is securely handled and stored.
Reduced Administrative Costs: Digital systems decrease the need for paper forms and physical storage, leading to long-term savings.
Scalable for Different Practice Sizes: Digital check-in systems can be scaled up or down depending on the needs of the facility, from small practices to large hospitals.
Types of Digital Patient Check-In Solutions
Web-Based Solutions:
Patients can access the check-in system via a website link or patient portal.
Ideal for remote check-ins and can be used on any internet-enabled device.
Mobile Apps:
A dedicated app allows patients to check in, schedule appointments, receive reminders, and complete forms.
Enhances patient engagement and encourages repeat visits by improving convenience.
In-House Kiosks:
Patients can check in upon arrival at a physical kiosk or tablet station.
Useful for practices with high foot traffic, as it allows for faster patient processing.
Considerations for Implementing a Digital Check-In System
HIPAA Compliance: Ensure the system adheres to HIPAA standards to protect patient privacy and data security.
User-Friendly Interface: Choose an intuitive and easy-to-navigate system for patients of all ages and tech abilities.
Customization Options: Ensure the system allows for customizable forms, fields, and check-in workflows to match practice requirements.
Integration Capabilities: Opt for a system that integrates with your EHR, billing, and appointment scheduling software.
Technical Support and Training: Choose a patient engagement software vendorsthat offers comprehensive support, training, and troubleshooting for seamless implementation.
Popular digital patient check in Software Options
Phreesia: Known for its extensive features, including digital forms, insurance verification, and integration with various EHR systems.
Solutionreach: Offers check-in, reminders, and two-way communication between patients and healthcare providers.
Kareo: A versatile option for smaller practices with features for intake, scheduling, and EHR integration.
ModMed: Specializes in digital check-ins and telehealth services for specialty practices, particularly dermatology and orthopedics.
Clearwave: Provides streamlined digital check-in solutions with a focus on patient self-service and multi-site practices.
A digital check-in system can significantly improve operational efficiency, streamline administrative tasks, and enhance the overall patient experience. If you’re considering implementing a system, I can provide more specific recommendations based on the needs of your practice.
An electronic patient check-in system digitizes the process of patient arrival and data entry at healthcare facilities, streamlining check-ins and improving the flow of information. This approach has become popular for its efficiency, ease of use, and ability to integrate seamlessly with Electronic Health Records (EHR) and billing systems. Here’s a breakdown of electronic patient check-in systems, their features, and their benefits:
Key Features of an Electronic Patient Check-In System
Self-Service Check-In:
Patients can check in themselves at kiosks or on their mobile devices, entering or verifying their information directly.
Reduces the need for front desk involvement, speeding up the process.
Mobile and Web Check-In Options:
Patients can check in remotely via a mobile app or a secure web link before arriving.
Reduces wait times and allows for better planning of patient flow in the office.
Pre-Appointment Form Completion:
Patients fill out medical histories, consent forms, and other necessary documents before arrival.
Ensures records are updated and readily available for the healthcare provider.
Insurance Verification and Co-Pay Collection:
Checks insurance eligibility and allows co-pays to be collected electronically, either before or at the time of check-in.
Reduces back-office work and minimizes billing delays.
Symptom and Health Screening:
Customizable health questionnaires can collect symptom information or screen for specific conditions (e.g., COVID-19).
Allows for safer, more efficient triage and prepares providers in advance.
E-Signature for Consent and Compliance:
Collects electronic signatures for required documents such as consent, privacy policies, and financial agreements.
Provides legal compliance with fewer paper forms.
Appointment and Queue Management:
Patients receive estimated wait times and updates about their position in the queue.
Helps manage patient flow and reduces overcrowding in waiting areas.
Data Synchronization with EHR and PMS:
Automatically updates the Electronic Health Record (EHR) and Practice Management System (PMS) with patient data.
Provides clinicians with real-time access to updated patient information.
Multi-Language Support:
Supports multiple languages, enhancing accessibility for diverse patient populations.
Improves patient experience and comprehension for non-native speakers.
Compliance with Privacy Regulations:
Ensures secure storage and transmission of patient data in line with HIPAA and other regulatory standards.
Incorporates data encryption, secure logins, and limited access to sensitive information.
Types of Electronic Patient Check-In Systems
Mobile-Based Check-In:
Patients use a mobile app or a web portal for check-in, typically linked to the healthcare provider’s system.
Allows remote check-in and form completion before arrival, reducing in-office wait times.
Kiosk-Based Check-In:
Patients use an on-site kiosk or tablet, scanning an ID or entering their details upon arrival.
Ideal for facilities with high patient volumes, as it automates the intake process and minimizes front desk tasks.
Hybrid Systems:
Combines mobile and kiosk options, giving patients flexibility to check in remotely or upon arrival.
Offers a more comprehensive solution for practices of varying sizes.
Benefits of an Electronic Patient Check-In System
Streamlined Operations: Reduces paperwork and administrative tasks, allowing staff to focus on patient care.
Enhanced Patient Experience: Improves convenience and reduces waiting times, leading to greater patient satisfaction.
Improved Data Accuracy: Direct patient entry of data minimizes the risk of errors and reduces redundancies.
Secure and Compliant: Ensures that sensitive patient information is securely managed, stored, and accessed.
Reduced Costs: Minimizes the need for paper forms, filing, and physical storage, saving on materials and time.
Scalability: These systems can scale to fit the needs of small practices, large hospitals, or multi-site facilities.
Popular Electronic Patient Check-In Solutions
: Known for robust self-service capabilities, Phreesia offers tools for patient check-in, payment processing, and data integration with EHRs.
IntakeQ: Offers HIPAA-compliant forms, online check-in, and secure data handling, making it popular with small to mid-sized practices.
SimplePractice: A versatile patient intake management software option with electronic check-in, telehealth integration, and EHR features tailored for smaller practices.
Kareo: Provides all-in-one features that include patient check-in, billing, and EHR integration, suitable for smaller healthcare providers.
Clearwave: Specializes in self-service check-in and patient engagement software for larger, multi-location practices, helping to streamline high patient volumes.
Considerations for Implementing an Electronic Check-In System
User Friendliness: Ensure the system is intuitive and accessible for all patient demographics, including those who may not be tech-savvy.
Compatibility with Existing Systems: Choose software that integrates smoothly with your current EHR, billing, and appointment scheduling systems.
Compliance with Privacy and Security Standards: Verify that the system complies with HIPAA and other relevant privacy laws.
Customization: Look for a system that allows form customization, language options, and configurable check-in workflows.
Technical Support and Training: A good vendor should offer comprehensive support, training, and resources to help both patients and staff.
Automated patient intake systems digitize and streamline the entire process of gathering patient information, verifying insurance,
e steps, healthcare practices can improve efficiency, accuracy, and patient satisfaction, allowing patients to complete intake tasks on their own time, from any location, using web-based or mobile solutions.
A patient intake system streamlines the process of gathering and managing patient information before an appointment, typically using digital tools to enhance efficiency, data accuracy, and the overall patient experience. This type of system is especially useful for reducing paperwork, shortening wait times, and improving the accuracy of medical records by allowing patients to input data directly. Here’s an overview of the core features, benefits, and types of patient intake systems:
A patient check in app digitizes the arrival automated patient check in system process at healthcare facilities, allowing patients to check in, complete forms, verify insurance, and even make payments from their mobile device. These best patient intake softwareautomated patient check in system apps streamline the patient intake process, improve data accuracy, reduce wait times, and enhance the overall patient experience. Here’s a closer look at the features, benefits, and considerations for implementing a patient check-in app:
An automated patient check-in system streamlines the check-in process by using technology to handle routine administrative tasks, enabling patients to check in efficiently with minimal staff intervention. This type of system improves patient flow, reduces wait times, enhances data accuracy, and provides a more convenient experience for patients and staff alike.
There are several highly-regarded patient intake software for patient engagement options available, each offering unique features designed to improve the efficiency and effectiveness of the patient intake medical check in software process. Here are some of the best patient check in systems software solutions, highlighting their strengths and the types of healthcare practices they best serve:
Medical check-in software is designed to streamline the patient arrival process in healthcare facilities by automating tasks like form completion, insurance verification, and payments. These systems improve automated patient check in flow, reduce waiting times, enhance data accuracy, and allow staff to focus more on patient care rather than administrative tasks. Here are some of the top medical check-in software solutions, including their key features, benefits, and ideal practice settings:
Medical check-in best patient engagement software is designed to streamline the patient arrival process in healthcare facilities by automating tasks like form completion, insurance verification, and payments. These systems improve patient self check in flow, reduce waiting times, enhance data accuracy, and allow staff to focus more on patient care rather than administrative tasks. Here are some of the top medical check-in software solutions, including their key features, benefits, and ideal practice settings:
what is patient engagement software
Online patient intake software allows healthcare practices to collect patient self check in system information digitally before or during their visit. This can be done through web portals, mobile apps, or email links, helping to streamline the intake process. online patient intake software intake software typically includes forms for personal, medical, and insurance details, as well as features for e-signatures, consent collection, insurance verification, and payment processing. It’s particularly beneficial for reducing paperwork, enhancing patient experience, and improving data accura
Patient intake management software is designed to help healthcare practices streamline and automate the intake process, from the moment a patient schedules an appointment to when they complete all necessary forms, verify their insurance, and make payments. This type of urgent care patient engagement software typically includes features such as customizable forms, e-signatures, insurance verification, patient communications, and integration with EHR/Practice Management systems.
Patient intake management software is designed to help healthcare practices streamline and automate the intake process, from the moment a patient schedules patient engagement software pricing an appointment to when they complete all necessary forms, verify their insurance, and make payments. This type of software typically includes features such as customizable forms, e-signatures, insurance verification, patient communications, and integration with EHR/Practice Management systems.
patient payment software refers to digital patient engagement software check in tools and platforms designed to enhance communication, interaction, and overall involvement of patients in their healthcare journey. These patient engagement software solution focus on improving the patient experience by offering features such as appointment scheduling, reminders, telemedicine, patient engagement software companies education, and personalized care plans, while fostering stronger relationships between patients and providers. Engaging patients throughout their healthcare process can lead to better outcomes, improved patient satisfaction, and more efficient practice operations.
Hospital patient payment software is designed to streamline the process of collecting electronic patient check in, reducing administrative overhead, and improving revenue cycle management. These dental patient engagement software systems can handle everything from co-pays and patient engagement software solutions deductibles to patient balances and insurance claims, making it easier for hospitals to process payments, improve cash flow, and enhance the patient experience.
Integrated patient payment software refers to systems that seamlessly connect with a healthcare provider's existing EHR (Electronic Health Record), EMR (Electronic Medical Record), practice management software, and revenue cycle management (RCM) tools to streamline the entire billing and payment process. These systems automate the patient payment experience, allowing for real-time tracking of patient balances, offering online payment portals, and integrating billing information into clinical trial patient engagement software workflows. The integration ensures smooth data flow between clinical, administrative, and financial departments, improving operational efficiency and patient satisfaction.
Automated patient payment software is designed to simplify and streamline the entire billing and payment process for healthcare providers and patients. These platforms automate various aspects of the payment cycle, including sending payment reminders, processing online payments, offering payment plans, and integrating seamlessly with Electronic Health Record (EHR) and Revenue Cycle Management (RCM) systems. The goal is to reduce administrative burden, accelerate payment collections, and enhance the patient experience by providing an easy and efficient way to manage their medical bills.
0 notes
Text
Emerging Trends in Hospital Billing for 2024 and Beyond
In an ever-evolving healthcare landscape, hospital billing services play a pivotal role in ensuring the financial stability of healthcare institutions. The year 2024 brings exciting advancements and emerging trends aimed at improving efficiency, accuracy, and patient satisfaction. These trends highlight the importance of reliable hospital billing services and how providers like Medi Claim Management can help healthcare organizations thrive.
Advanced Automation in Medical Billing Services
Automation continues to revolutionize the field of medical billing and coding. In 2024, healthcare providers are increasingly adopting AI-driven tools to streamline repetitive tasks like data entry, insurance claim processing, and denial management.
This shift towards automation reduces errors, enhances efficiency, and speeds up revenue cycle management. Tools like predictive analytics are also being used to identify patterns in claims denials, allowing proactive resolution before submission. Medi Claim Management leverages cutting-edge technology to provide hospitals with automated solutions that ensure timely and accurate billing, freeing up staff to focus on patient care.
Increased Focus on Patient-Centric Billing
Patients today demand transparency in billing and a simplified process for payments. Hospital billing services must now include features like online payment portals, clear itemized bills, and real-time assistance.
In 2024 and beyond, patient-centric billing will be a key differentiator for healthcare providers. Medi Claim Management excels in offering billing solutions that enhance patient satisfaction, from simplified insurance claim processing to easy payment options. By putting patients at ease, hospitals can foster trust and long-term loyalty while ensuring timely collections.
Integration of Revenue Cycle Management with EHR Systems
The integration of electronic health records (EHR) with revenue cycle management (RCM) systems is becoming a game-changer in hospital billing. This seamless connection ensures better data sharing, accurate billing codes, and quicker claims management services.
For example, real-time updates from EHRs can help reduce claim rejections due to coding errors. Medi Claim Management specializes in integrated hospital billing services that connect RCM workflows with existing hospital systems, ensuring smooth operations and enhanced cash flow.
Enhanced Compliance and Data Security
With the rise of cyber threats and regulatory changes, data security and compliance are top priorities in hospital billing services. Hospitals need to adhere to stringent regulations like HIPAA while ensuring sensitive patient data is secure during medical billing and coding processes.
In 2024, advanced encryption and blockchain technology are emerging as key solutions. Medi Claim Management offers hospital billing services designed to prioritize compliance and protect sensitive data, giving hospitals peace of mind while optimizing their claims processing.
Outsourcing for Efficiency and Cost Reduction
As billing processes become more complex, many hospitals are turning to outsourcing medical billing services to save costs and improve efficiency. By partnering with specialists like Medi Claim Management, hospitals can focus on core healthcare services while experts handle claims management services and insurance claim processing.
Outsourcing ensures access to a skilled team, up-to-date knowledge of industry regulations, and cutting-edge technology, all of which contribute to faster reimbursements and minimized errors.
Why Medi Claim Management Is Your Ideal Partner
As hospital billing evolves, having a reliable partner for medical billing and coding is more critical than ever. Medi Claim Management offers:
Comprehensive Hospital Billing Services: Tailored solutions to meet your specific needs.
Claims Management Expertise: Ensuring maximum approval rates and minimal denials.
Revenue Cycle Optimization: Streamlined processes to boost cash flow.
Patient-Centric Approach: Enhancing satisfaction while improving collections.
In 2024 and beyond, hospitals need partners that understand the challenges of modern billing and provide solutions that drive results. Medi Claim Management combines technology, expertise, and a commitment to excellence, making it the go-to choice for hospital billing services.
Conclusion
Emerging trends like automation, patient-centric billing, and seamless RCM integration are shaping the future of hospital billing services. By staying ahead of these trends, hospitals can ensure financial stability and better patient outcomes.
Partnering with Medi Claim Management means accessing state-of-the-art medical billing services designed to simplify insurance claim processing, improve revenue cycle management, and deliver exceptional results. Ready to take your hospital billing to the next level?
Contact us today for a free consultation and discover how we can transform your financial operations.
#medical billing services#hospital billing services#claims management services#medical billing and coding#insurance claim processing#healthcare#health#revenue cycle management
0 notes
Text
Learning Medical Billing and Transcription: Essential Strategies for Success in Healthcare
Mastering Medical Billing and Transcription: Essential Strategies for Success
Mastering Medical Billing and Transcription: Essential Strategies for Success in Healthcare
The healthcare industry is a complex ecosystem where every detail matters, particularly in medical billing and transcription. These two components are vital for ensuring smooth operations, accurate patient records, and timely reimbursement from insurance providers. In this article, we’ll explore essential strategies for mastering medical billing and transcription, providing practical tips that can significantly elevate your practice.
Understanding Medical Billing and Transcription
Before delving into strategies, it’s crucial to understand what medical billing and transcription entail:
Medical Billing
Medical billing is the process of submitting and following up on claims with health insurance companies to receive payment for services rendered by healthcare providers. This includes:
Charge entry
Claim submission
Payment posting
Accounts receivable management
Medical Transcription
Medical transcription involves converting voice-recorded reports from physicians into written text. It requires:
Accurate listening and typing skills
Understanding of medical terminology
Knowledge of relevant guidelines and standards
Benefits of Mastering Medical Billing and Transcription
Mastering these processes offers numerous advantages:
Improved Revenue Cycle Management: Efficient billing processes lead to faster payments.
Enhanced Patient Care: Clear and accurate transcription ensures better patient history and treatment continuity.
Reduced Errors: Proper training and management can minimize mistakes, thus preventing revenue loss and legal issues.
Increased Productivity: Streamlined processes save time for healthcare providers, allowing them to focus more on patient care.
Essential Strategies for Success
1. Invest in Comprehensive Training
The foundation of successful medical billing and transcription lies in thorough training. Consider the following:
Enroll in accredited courses that cover both billing and transcription.
Utilize online platforms that offer continuing education credits.
Engage in workshops and seminars to stay updated on industry trends.
2. Utilize Advanced Technology
Harnessing technology can streamline both billing and transcription processes. Here are some tools to consider:
Billing Software: Use reputable medical billing software to automate claims processing.
Transcription Tools: Implement voice recognition software to improve efficiency in transcription tasks.
Data Management Systems: Consider integrated systems that combine billing and patient management for holistic operation.
3. Understand Coding Systems
A solid understanding of medical coding (ICD, CPT codes) is essential. This will aid in:
Ensuring accurate billing
Facilitating correct claims submissions
Reducing claim denials due to coding errors
4. Foster Clear Communication
Effective communication between healthcare providers and billing professionals is critical. Implement strategies such as:
Regular meetings to review billing protocols.
Creating a feedback loop for questions and concerns regarding patient information.
Case Study: Success through Training and Technology
One healthcare clinic in California reported a 30% increase in its revenue cycle efficiency after investing in an extensive training program and upgrading its billing software. The clinic focused on:
Training all staff on latest ICD-10 updates.
Implementing an intuitive and automated billing system.
Scheduling regular follow-ups on outstanding claims.
As a result, the clinic not only reduced its claim turnaround time but also enhanced patient satisfaction due to timely billing explanations.
Firsthand Experience: The Importance of Accurate Transcription
In my years as a medical transcriptionist, I’ve witnessed firsthand the challenges posed by inaccurate transcriptions. One notable instance involved a misinterpreted medication dosage that led to a patient receiving incorrect treatment. This highlighted the dire need for diligence in transcription tasks.
Lessons learned include:
Always verify unclear audio with the healthcare provider.
Utilize reliable reference materials for medical terminology.
Engage in ongoing education for constant skill improvement.
Best Practices in Medical Billing and Transcription
Here are some best practices to follow:
Practice
Description
Double-Check Claims
Review all claims before submission for accuracy.
Establish a Follow-Up Routine
Set a timeline for following up on unpaid claims.
Maintain Patient Privacy
Always comply with HIPAA regulations in all documentation.
Conclusion
Mastering medical billing and transcription is no small feat, but with the right strategies, training, and technology, it can significantly enhance healthcare operations. By investing in learning, utilizing technology, and maintaining effective communication, healthcare entities can improve their revenue cycles, reduce errors, and ultimately provide better patient care. The journey may have its challenges, but the benefits of efficient billing and accurate transcription are invaluable. Start implementing these essential strategies today and watch your practice thrive in the evolving healthcare landscape.
youtube
https://medicalbillingcodingcourses.net/learning-medical-billing-and-transcription-essential-strategies-for-success-in-healthcare/
0 notes
Text
Unlocking Potential with Back Office Outsourcing

Today, achieving operation efficiency is not a choice but a must in today's dynamic business world. From cost-cutting to increasing productivity, firms embrace outsourced back office services as the enabler in ensuring competitiveness. Companies will be able to streamline operations, open growth possibilities, and refocus on core activities by aligning with industry leaders like OnestopDA.
This blog goes closer to discussing the strengths in back office outsourcing services and penetrates two specific positions that really typify what has been achieved in outsourcing: the Medical Executive Assistant and the Logistics Administrative Assistant.
What are Back Office Outsourcing Services?
Back-office outsourcing is when a firm delegates non-statutory as well as not client-facing operations to third-party experts. It ranges from data entry, payroll, bookkeeping, all other general administrative work, all the way to IT support.
Companies, such as OnestopDA, are specializing in back office outsourcing to ensure that companies can receive effective, reliable, and cost-effective solutions specific to their needs.
Critical Advantages of Back Office Outsourcing
Cost Efficiency
In-house back office teams are usually expensive. Outsourcing with the best back office outsourcing companies like OnestopDA helps save employee salaries, training, and infrastructure.
Enhanced Productivity
Outsource redundant tasks to a professional back-office company and liberate your team to concentrate on strategic efforts, thus enhancing overall productivity.
Expertise at Your Fingertips
Access to special knowledge and the most modern tools for the best results is given by outsourced back-office services.
Scalability
It is flexible in scale operations as business demands change, making the system the most important asset for businesses of all sizes, as it scales operations.
Medical Executive Assistant: Streamlining Healthcare Operations
In the health sector, efficiency is paramount. A Medical Executive Assistant acts as a vital communication link between service providers, patients, and managerial processes.
Outsourcing this role to experienced professionals such as OnestopDA can benefit healthcare organizations in several ways:
Improve Patient Care: A Medical Executive Assistant manages appointment scheduling, billing, and records-keeping, enabling physicians to spend quality time with patients.
Improve Compliance: The professionals outsourced are abreast of medical regulations, so adherence to legal standards is guaranteed.
Reduce Administrative Load: Healthcare providers can outsource time-consuming tasks for efficient performance.
Logistics Administrative Assistant: Maximizing Supply Chain Management
For companies requiring a complex supply chain, companies require a Logistics Administrative Assistant to govern shipments, handle inventories, and ensure smooth communication at all points of the chain.
Many organizations' benefits of outsourcing this role include:
Smooth Operations: A Logistics Administrative Assistant ensures timely delivery and efficiency in workflow.
Cost Efficiency: Outsourcing saves overheads in hiring and training in-house personnel.
Agility: Expert professionals make better adjustments to an interruption that quickly keeps the operations on track.
Why outsource to OnestopDA?
OnestopDA is one of the most nimble back office outsourcing companies dedicated to customized solutions that lead to success. From Medical Executive Assistants to Logistics Administrative Assistants, OnestopDA makes sure to meet your operational needs with precision.
Tailored Services: Solutions aligned with your business objectives.
Expert Teams: Highly experienced professionals who have domain-specific knowledge.
Advanced Tools: State-of-the-art technologies to deliver smooth operations.
Back Office Outsourcing: Game-changer in Businesses
Operational excellence is not an exercise in cost cutting; rather, it aims at unshackling the whole business potential. Back office outsourcing services are the perfect response of organizations that are opting for growth in the most efficient and effective manner.
Business operations can be streamlined and even made more accurate and efficient by outsourced roles such as the Medical Executive Assistant and the Logistics Administrative Assistant.
Partner with the Best: OnestopDA
Whatever your needs are, if it's either in daily errands or specialized administrative work, OnestopDA will be there for you. With their expertise in outsourced back office services including Medical Executive Assistants and Logistics Administrative Assistants, rest assured that you will get the best support.
Discover how OnestopDA's back office outsourcing services can transform your operations. Contact them today and take the first step toward operational excellence!
#backoffice#backofficeservice#back office outsourcing#outsourced back office service#healthcare#medical executive assistant#logistics#longistics assistant#healthcare assistant#onestopda#virtual assistant#administrative assistance#virtual assistance services#service#virtual service
0 notes
Text
Boost Efficiency with EMR System Integration and Cardiology Billing Services

In the dynamic world of healthcare, efficiency and accuracy are the cornerstones of successful practice management. One of the key ways to achieve this is through EMR system integration, which seamlessly connects all aspects of patient data, billing, and operational processes. At Billing Paradise, we provide cutting-edge solutions that streamline your workflows and improve your financial performance.
Why EMR System Integration is Essential
EMR system integration is no longer just a convenience; it is a necessity for healthcare providers aiming to improve operational efficiency. By integrating charge capture software directly into your electronic medical records (EMR) system, you can minimize errors, enhance data accuracy, and reduce delays in claim submissions. This streamlined process ensures that healthcare providers can focus more on patient care and less on administrative burdens.
Our embedded charge capture software works seamlessly with your EMR system, allowing providers to capture charges in real-time, reduce missed revenue opportunities, and accelerate the reimbursement cycle. This solution is particularly valuable for specialties like cardiology, where billing complexities often result in claim denials and delays.
The Impact of EMR Integration on Cardiology Practices
For cardiology practices, integrating your EMR system with specialized billing tools is critical. The field of cardiology often involves complex coding, procedure-specific billing, and frequent insurance updates. Our cardiology billing services are designed to handle these challenges effectively, ensuring that your practice's revenue cycle remains robust and compliant.
Explore more about our cardiology billing services, which focus on precision and compliance while maximizing revenue opportunities. These services ensure that cardiology practices can focus on delivering exceptional patient care without worrying about the intricacies of billing and coding.
Key Benefits of EMR System Integration
Enhanced Data AccuracyIntegration eliminates manual data entry errors, ensuring accurate patient records, billing details, and claims submissions.
Streamlined WorkflowsBy integrating all your systems, from scheduling to billing, your staff can operate more efficiently, reducing bottlenecks in administrative processes.
Improved Revenue CaptureEmbedded charge capture ensures that no billable services are overlooked, maximizing your practice's revenue potential.
Faster Reimbursement CyclesAccurate and timely claim submissions result in quicker reimbursements, improving cash flow for your practice.
Regulatory ComplianceIntegrated systems are better equipped to handle regulatory updates, ensuring that your practice remains compliant with the latest industry standards.
Why Choose Billing Paradise
At Billing Paradise, we specialize in providing tailored solutions that meet the unique needs of healthcare providers. Whether it's EMR system integration or cardiology billing services, our team of experts ensures that your practice operates at peak efficiency.
Additionally, our blog on embedded charge capture software offers insights into how this technology can revolutionize your billing process. It is a must-read for healthcare providers looking to improve their financial outcomes through technology.
The Role of Cardiology Billing Services
Our cardiology billing services are specifically designed to address the challenges unique to cardiology practices. With expertise in complex coding and regulatory compliance, we ensure accurate claim submissions and minimal denials. These services include:
Comprehensive charge capture for cardiology-specific procedures
Expert coding for complex interventions
Proactive denial management to reduce revenue leakage
Regular updates on payer guidelines and regulatory changes
How EMR Integration and Billing Services Work Together
The combination of EMR system integration and specialized billing services creates a powerful ecosystem for healthcare providers. Integration ensures that all data flows seamlessly between systems, while expert billing services handle the nuances of coding and claims management. This synergy leads to better financial outcomes and improved patient care.
Take the Next Step
Don’t let outdated processes hold your practice back. Embrace the power of EMR system integration and specialized billing services to transform your operations. Visit our dedicated pages on embedded charge capture software and cardiology billing services to learn more about how these solutions can benefit your practice.
Conclusion
In today’s healthcare landscape, efficiency and accuracy are critical for success. With EMR system integration and expert cardiology billing services, you can ensure that your practice operates smoothly, stays compliant, and maximizes revenue. Billing Paradise is your trusted partner in achieving these goals. Let us help you navigate the complexities of healthcare billing and optimize your revenue cycle for sustained success.
0 notes
Text

Apply Road Accident Fund (RAF) x17 Admin Vacancies Road Accident Fund (RAF) x17 Admin Vacancies The Road Accident Fund (RAF), a cornerstone of road safety and financial assistance in South Africa, is hiring Administrative Assistants for its Claims division. With 17 positions available in various departments, this opportunity offers an exciting platform for skilled individuals to contribute to a vital organization while gaining invaluable experience. This role, offered on a 12-month fixed-term contract, is based in Cape Town, Western Cape. - Job Title: Administrative Assistant - Division: Claims - Reference No: 5076 - Location: Cape Town, Western Cape - Contract Type: Fixed-Term Contract (12 months) - Salary: R244,732.00 per annum - Grade: T.A.S.K Grade 06 - Application Deadline: 3 December 2024 - Employment Equity: Not a disability-targeted role Departmental Openings The 17 positions are distributed across the following departments: - Onboarding Department: 4 positions - Adjudication Department: 4 positions - Legal Admin Department: 7 positions - Medical Management Department: 2 positions The Administrative Assistant will support day-to-day operations across various departments, ensuring smooth workflows and compliance with organizational standards. Key Responsibilities 1. Compliance Administration - Maintain updated documentation and ensure compliance with RAF policies. - Adhere to internal control measures and organizational objectives. - Ensure proper record-keeping to support departmental audits. 2. Office Coordination - Manage correspondence, filing, and telephonic inquiries. - Maintain strict confidentiality in all departmental matters. - Ensure timely responses to requests and organize documentation. - Validate documents for accuracy and prevent duplicate entries. 3. Meeting Support - Arrange and confirm meetings for departmental stakeholders. - Record, compile, and distribute minutes following governance standards. - Maintain team diaries and appointment schedules. 4. Document and Records Management - Administer proper record-keeping and filing per RAF guidelines. - Secure delivery of documents and ensure accurate data capturing. Qualifications and Experience To qualify for the Administrative Assistant position, candidates must meet the following requirements: - Educational Requirement: Matric or Grade 12 Certificate - Experience: At least 1 year in an administrative or similar role Skills and Competencies Technical Skills - Proficiency in MS Word, Excel, and PowerPoint. - Solid administrative and organizational capabilities. - Basic understanding of Supply Chain Management (SCM) and financial principles. Behavioral Skills - Strong planning and coordination abilities. - High ethical standards and emotional intelligence. - Exceptional verbal and written communication skills. - Excellent client service orientation. Core Values at RAF As an integral part of the RAF team, you will embody the organization’s core values: - Integrity: Upholding honesty and transparency in all operations. - Compassion: Providing empathetic service to road accident victims. - Accountability: Taking responsibility for your work and decisions. - Respect: Treating all individuals with dignity and fairness. - Excellence: Striving for the highest standards in service delivery. SEE ALSO: Rand Water x19 Senior Engineer Technologist 2024 How to Apply? Click Here to Apply Read the full article
0 notes
Text
Labcorp Clinical Report Writer Coordinator Job Vacancies Labcorp, a global leader in life sciences and healthcare solutions, is hiring a Clinical Report Writer Coordinator in Bangalore, India. This entry-level position offers an exciting opportunity to develop expertise in clinical trial documentation, working within a dynamic team environment. If you have a passion for clinical writing and are ready to kick-start your career, this role is for you! Labcorp Hiring Clinical Report Writer Coordinator Labcorp is actively seeking a dedicated and detail-oriented individual to join their LMVRS (Labcorp Medical Writing and Reporting Services) team. As a Clinical Report Writer Coordinator, you will contribute to producing high-quality clinical trial documentation that supports research and innovation in healthcare. Key Job Details Job Title: Clinical Report Writer Coordinator I Category: Clinical Location: Bangalore, India Job ID: 2444315 Job Type: Full-Time Job Responsibilities As a Clinical Report Writer Coordinator, you will: The Report Writer Coordinator is an entry level position in the LMVRS group, learning the Labcorp writing standard and learning to draft and edit reports to promote product consistency. Learns to use software tools to efficiently and accurately complete job duties. Learns and understands any new/changed conventions or standard language. Creates report folders and requests all needed information, documentation and any other relevant information from the respective departments. Creates part of the initial draft of lower complexity clinical trials internal or client facing documents using pre-defined templates or client-supplied information with guidance from more senior colleagues and using study protocol information, SOPs and/or lab data. Creates data tables, as needed, using the corresponding database(s). Performs review and quality control (QC) as applicable. Edits internal or client facing documents, as needed, after review, ensuring that company convention, style, format and terminology have been used. Independently utilizes workload management tool to track and document data and report completion activities. Ensures compliance to applicable departmental Standard Operating Procedures and Work Instructions. Maintains/develops training manuals. Effectively manages own time and deadlines. Effectively manages task status tracking and time recording. May provide backup assistance to colleagues, as appropriate. Performs other duties as assigned. [caption id="attachment_111808" align="aligncenter" width="1200"] Labcorp Hiring Clinical Report Writer Coordinator – Entry-Level Opportunity in Bangalore[/caption] Eligibility Criteria To apply for this role, candidates must possess: Strong writing and communication skills. Proficiency in using software tools for data management and document creation. Excellent time management abilities. This position is ideal for individuals eager to grow in the field of clinical writing within a supportive and innovative organization. How to Apply To apply for the Clinical Report Writer Coordinator role, visit the official Labcorp careers page at the link below: Apply Here Equal Opportunity Employer Statement Labcorp is proud to be an Equal Opportunity Employer. Employment decisions are based on qualifications and business needs, without discrimination based on race, gender, religion, or other protected characteristics.
0 notes