#H2 Receptor Blockers
Explore tagged Tumblr posts
Note
If you feel like talking about it — what’s the *aftermath* of anaphylaxis like? I know that an epipen is just step one, and further treatment and observation follows at a hospital, but I’m curious about what the subjective experience is like in the longer term; whether one can bounce back fairly well or whether there’s lingering unpleasantness.
So with the caveat that everyone experiences things differently (and putting this under a cut because I don't want to trigger anyone):
After epi is administered, you're usually put on a cocktail of drugs ranging from several different IV antihistamines (typically a mix of h1 and h2 histamine blockers and a giant whack of benadryl), anti-nausea meds, a beta-agonist to assist with breathing, and a shit-whack of steroids.
Once you've been stable for a few hours and discharged, you'll be told to watch for symptoms for up to 72 hours, which is the period in which a biphasic reaction can happen. (For me, it's always within 20 minutes to 8 hours after rescue medication is administered if I'm going to slip back into an allergic response, but everyone is different.)
Depending on your symptoms, you'll sometimes be told to take an antihistamine for up to 72 hours (if you're not already taking one daily), but the one thing they always send you home with is a steroid like prednisone. I usually need a 5-7 day dose because I need to taper off it or my adrenals crash, but some people get a 3-day dose and come off it with no problems.
Body-wise, it's a draining experience, and the medications often leave you both tired and wired. It's an odd sensation.
Mentally and emotionally, it takes me a lot longer to recover because I've just been smacked with a proverbial mallet of stress hormones and adrenaline, and that can often lead to depressive moods and even rage for some people. The prednisone also heightens emotions, so it's not unusual to be having some of the wildest mood swings of your life while also processing the stress of what just happened.
It takes me a while to bounce back, typically about a week on full rest, but I know some people who claim to feel fine in a couple of days. Couldn't be me, haha. My body goes into hibernation mode for quite a while, and I'll be lying in bed exhausted and jittering like I've had ten espressos, but I don't know how much of that is general anaphylaxis or how much of that is specific to my mast cell disorder.
So, for me, it's a desperate need to sleep, jitteriness, depression, and rapid mood swings from the prednisone followed by a general feeling of blegh. It also takes me about 72 hours to be able to eat solid foods again because of the effect anaphylaxis has on the digestive tract (the esophagus is lined with histamine receptors; that's why some heartburn meds are actually antihistamines.), but I suspect that's my MCAS.
It's basically just a bit shit, lol.
830 notes
·
View notes
Text
What is Idiopathic Mast Cell Activation Syndrome?
Idiopathic Mast cell activation syndrome (MCAS) is one of several mast cell disorders. MCAS occurs when there are a normal number of mast cells in a person's body but they over-release mast cell mediators causing random allergic reactions in multiple systems of the body. MCAS is incredibly common being present in an estimated 17% of the population.
Symptoms
MCAS symptoms are incredibly varied and always occur in multiple systems of the body. Anaphylaxis is common.
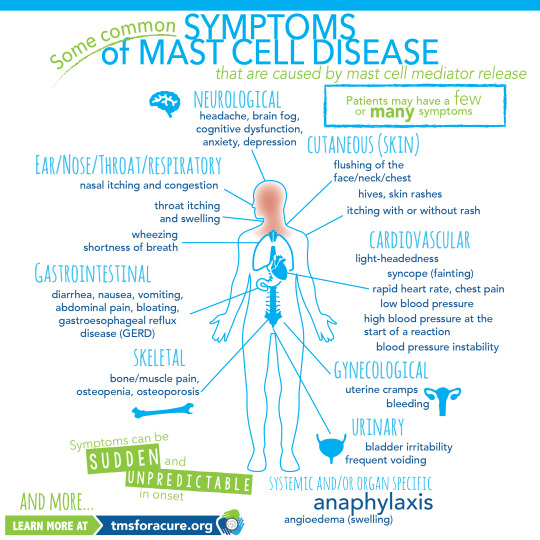
[ID: A graphic labeled "Some common symptoms of Mast Cell Disease" A graphic of a person standing in the center with multiple organs visible is shown. Around the person are lines pointing to specific areas of the body labeled with the body system and symptoms. Clockwise these read "Neurological headache, brain fog, cognitive dysfunction, anxiety, depression Cutaneous (Skin) flushing of the face/neck/chest, hives, skin rashes, itching with or without rash Cardiovascular light-heartedness, syncope (fainting), rapid heart rate, chest pain, low blood pressure, high blood pressure at the start of a reaction, blood pressure instability Gynecological uterine cramps, bleeding Urinary bladder irritability, frequent voiding Systemic and/or organ specific Anaphylaxis angioedema (swelling) Skeletal bone/muscle pain, osteopenia, osteoporosis Gastrointestinal diarrhea, nausea, vomiting, abdominal pain, bloating, gastroesophageal reflux disease (GERD) Ear/Nose/Throat/Respiratory nasal itching and congestion, throat itching and swelling, wheezing, shortness of breath and more" In the bottom left corner "Symptoms can be sudden and unpredictable in onset learn more at tmsforacure.org"]
MCAS symptoms are specifically not allergies. the reactions may look like allergies but the two are not the same and MCAS is not a condition meaning "many allergies" While MCAS can have some consistent triggers one of the defining features of the disease is that reactions are random and happen unpredictably.
Anaphylactic shock is not a requirement for diagnosis.
Diagnosis
MCAS is diagnosed by an immunologist. It is in part a diagnosis of exclusion and requires ruling out both allergies and systemic mastocytosis as well as other conditions such as certain types of tumors.
Diagnostic criteria for MCAS is debated. Some immunologists follow the symptom-based diagnosis approach in which case the diagnostic criteria are:
Recurring and severe anaphylactic-like episodes that involve more than one organ system
and
Positive response to mast cell stabilizing or mediator medications anaphylaxis-type symptoms
Others follow diagnostic criteria based on laboratory findings. In this case the diagnostic criteria are:
Episodic symptoms consistent with mast cell mediator release affecting two or more organ systems evidenced as follows:
Skin: urticaria, angioedema, flushing
Gastrointestinal: nausea, vomiting, diarrhea, abdominal cramping
Cardiovascular: hypotensive syncope or near syncope, tachycardia
Respiratory: wheezing
Naso-ocular: conjunctival injection, pruritus, nasal stuffiness
and
A decrease in the frequency or severity; or resolution of symptoms with anti-mediator therapy: H1 and H2 histamine receptor antagonists, anti-leukotriene medications (cysLT receptor blockers or 5-LO inhibitor), or mast cell stabilizers (cromolyn sodium)
and
Evidence of an elevation in a validated urinary or serum marker of mast cell activation: Documentation of elevation of the marker above the patient’s baseline during a symptomatic period on at least two occasions; or if baseline tryptase levels are persistently >15ng, documentation of elevation of the tryptase above baseline on one occasion. Total serum tryptase is recommended as the markers of choice; less specific (also from basophils) 24 hour urine histamine metabolites, or 11-beta-prostaglandin F2.
and
Primary (clonal) and secondary disorders of mast cell activation ruled out.
These are not all proposed diagnostic criteria as the subject is heavily debated. Generally, a laboratory-confirmed MCAS diagnosis is considered more legitimate.
Treatment
MCAS is a very treatable condition. Generally treatment follows a path from antihistamines -> mast cell mediators -> biologics.
Epipens are given to MCAS patients with a history of anaphylaxis.
Antihistamines are divided into 2 categories: H1 antagonists and H2 antagonists. These categories are determined based on the histamine receptor each one targets.
H1 antagonists mostly deal with systemic and cutaneous symptoms. H1 antagonists are also further divided into first and second generation antihistamines. first generation antihistamines include diphenhydramine (Benadryl) and Hydroxyzine. These tend to cause drowsiness. With second generation H1 antagonists cause fewer side effects and include drugs like loratadine (Claritin) and cetirizine (Zyrtec)
H2 antagonists primarily affect the gastrointestinal tract and include medications like famotidine (pepcid)
Typically when treating MCAS a person will be put on both a second generation H1 antagonist and an H2 antagonist.
When antihistamines do not treat symptoms well enough the next step is a mast cell mediator. The most common mast cell mediator is cromolyn sodium which is available by prescription only. (this is technically available OTC but it is at 1/50th the dose used for MCAS) Mast cell mediators work by preventing the degranulation of mast cells in the first place.
When both antihistamines and mast cell mediators are insufficient someone with MCAS might be prescribed a biologic such as Xolair to treat their remaining symptoms.
Sources:
American Academy of Allergy, Asthma, and Immunology
Mast Cell Hope
Mast Cell Activation Syndrome: Proposed Diagnostic Criteria
#mast cell activation syndrome#mcas#mast cell disease#mast cell activation disorder#mcad#chronic illness#chronically ill#physical disability#physically disabled
82 notes
·
View notes
Text
Gastroenterology Drugs
Antacid Drugs -- treat heartburn -- neutralize acid from the stomach
Antibiotic Drugs -- treat gastrointestinal infections caused by bacteria -- not effective against viral infections
Antidiarrheal Drugs -- treat diarrhea -- slow peristalsis -- increase water absorption
Antiemetic Drugs -- treat nausea and vomiting -- treat motion sickness
Drugs for Gallstones -- dissolve gallstones -- used instead of surgical removal
H2 Blocker Drugs -- treat gastroesophageal reflux disease -- treat peptic ulcers -- block H2 receptors in the stomach -- H2 = histamine 2 -- H2 triggers the release of HCl
Laxative Drugs -- treat constipation -- soften stool -- add dietary fiber -- stimulate intestinal mucosa
Proton Pump Inhibitor Drugs -- treat gastroesophageal reflux disease -- treat peptic ulcers -- block final step in production of HCl
.
Patreon
#studyblr#notes#my notes#pharmacology#pharmacology notes#pharma#pharma notes#pharm#pharm notes#pharmacy#pharmacy notes#medical pharmacology#medications#medication notes#pharmacological sciences#biochemistry#chemistry#medical chemistry#medical biochemistry#health science#science#scienceblr#medblr#biological science#common medications#pharmacodynamics#pharmacokinetics#chemical agents#toxicology#med chem
24 notes
·
View notes
Text
Acid Reflux vs. GERD: Differences, Symptoms, Causes, and Treatments

Do you often experience a burning sensation in your chest or find yourself avoiding certain foods due to discomfort? These could be signs of acid reflux or GERD. While these periods are sometimes used interchangeably, they define different levels of a similar issue. Understanding the difference between acid reflux and Gastroesophageal Reflux Disease (GERD) is essential for proper management and treatment. Let’s explore deep into the causes, symptoms, and treatment options for both conditions, helping to take control of digestive health.
What is acid reflux?
Acid reflux happens when stomach acid flows back into the esophagus. This happens because the lower esophageal sphincter (LES), a muscle that closes off the stomach from the esophagus, weakens or relaxes at the wrong time. Occasional acid reflux is common and may be started by certain foods, stress, or overeating.
Key symptoms of acid reflux:
Heartburn: A burning sensation in the chest, usually after eating.
Regurgitation: A sour or bitter-tasting acid backing up into the throat or mouth.
Bloating and burping.
What is GERD?
GERD is a regular condition of acid reflux. It’s diagnosed when acid reflux happens more than twice a week or leads to complications like inflammation of the esophagus. Unlike occasional acid reflux, GERD requires long-term medical intervention.
Key symptoms of GERD:
Constant heartburn.
Difficulty swallowing.
Chronic cough or hoarseness.
Chest pain, especially when lying down.
Decay of tooth enamel due to acid exposure.
Acid reflux vs. GERD: Understanding the differences
The main difference between acid reflux and GERD lies in the frequency and severity of symptoms. Occasional acid reflux is manageable through lifestyle changes and over-the-counter medications. In contrast, GERD is more severe and constant and can lead to complications like Barrett’s esophagus or esophageal cancer if untreated.
Causes of Acid Reflux and GERD
Both conditions convey similar causes, but GERD usually affects long-term issues with the LES or other underlying conditions.
Common causes:
Overeating or lying down after meals.
Obesity.
Pregnancy.
Smoking.
Certain foods and beverages, such as spicy foods, citrus fruits, coffee, and alcohol.
Medications like aspirin or ibuprofen.
Risk factors
Some people are more prone to developing GERD due to:
Hiatal hernia (a condition where part of the stomach pushes through the diaphragm).
Endless stress.
Genetic predisposition.
Diagnosing acid reflux and GERD by a gastro surgeon in Ahmedabad
Proper diagnosis is essential for effective treatment. The best gastroenterologist in Ahmedabad may use the following methods:
Endoscopy: A flexible tube with a camera scans the esophagus for damage.
pH Monitoring: Measures acid levels in the esophagus over 24 hours.
Esophageal manometry: Tests the strength and coordination of esophageal muscles.
Barium swallow test: X-rays highlight abnormalities in the esophagus or stomach.
Treatment options for acid reflux and GERD by a gastroenterologist in Ahmedabad
Effective treatment requires a combination of lifestyle changes, medications, and, in severe cases, surgical interventions.
Lifestyle Changes
Dietary adjustments:
Avoid trigger foods like chocolate, spicy dishes, and fatty meals.
Opt for smaller, frequent meals instead of large ones.
Weight management:
Losing excess weight can greatly reduce pressure on the LES.
Elevate your sleeping position:
Use a wedge pillow to keep your upper body elevated, reducing nighttime reflux.
Quit smoking and limit alcohol:
These habits weaken the LES and increase acid production.
Avoid eating before bedtime:
Wait at least 2-3 hours after eating before lying down.
Medications
Antacids: Provide quick relief by neutralizing stomach acid.
H2 receptor blockers: Reduce acid production and provide longer-lasting relief.
Proton pump inhibitors (PPIs) Block acid production and allow damaged esophageal tissue to heal.
Prokinetics: Help the stomach empty faster to reduce reflux episodes.
Surgical choices by a gastro surgeon in Ahmedabad
For severe GERD, surgery may be necessary:
Fundoplication: Strengthens the LES by wrapping the upper stomach around it.
LINX device: A magnetic ring is placed around the LES to prevent acid reflux.
Complications of untreated GERD
Ignoring GERD symptoms can lead to serious health issues:
Esophagitis: Inflammation of the esophagus.
Barrett’s esophagus: A precancerous condition where esophageal cells change due to acid exposure.
Esophageal strictures: Narrowing of the esophagus due to scar tissue.
Esophageal cancer: Rare but potentially fatal if not diagnosed early.
When to see a gastro surgeon in Ahmedabad
Seek medical attention if you experience:
Severe or frequent heartburn.
Difficulty swallowing.
Chest pain mimicking a heart attack.
Vomiting blood or passing black stools.
Unintended weight loss.
Preventing Acid Reflux and GERD
Prevention strategies can greatly reduce symptoms and improve quality of life:
Stay active: Regular exercise helps digestion and weight management.
Hydrate smartly: Drink plenty of water, but avoid carbonated beverages.
Chew gum: Stimulates saliva production, neutralizing acid.
Wear loose clothing: Tight outfits can put pressure on your stomach, worsening symptoms.
Read More : https://anandgastrosurgeon.com/acid-reflux-vs-gerd-differences-symptoms-causes-and-treatments/
0 notes
Text
Top 5 Treatment Options After an Acid Reflux Diagnosis
Acid reflux, often regarded as a common digestive disorder, affects millions of individuals worldwide. Characterized by the backward flow of stomach acid into the esophagus, this condition leads to symptoms such as heartburn, regurgitation, and difficulty swallowing. Once diagnosed, understanding the various treatment options becomes crucial for managing the discomfort and preventing further complications. Here, we delve into the top five treatment options available for those facing an acid reflux diagnosis and treatment, exploring their effectiveness and potential benefits.

1. Lifestyle Modifications
One of the most effective approaches to managing acid reflux involves implementing lifestyle modifications. These changes can significantly alleviate symptoms and improve overall health. Adopting a diet rich in whole foods while avoiding trigger foods, such as spicy dishes, fatty meals, and caffeinated beverages, is often recommended. Additionally, smaller, more frequent meals can help prevent excessive stomach pressure, which contributes to reflux.
Furthermore, maintaining a healthy weight is a critical factor. Excess weight can place additional strain on the stomach, leading to increased acid production and reflux episodes. Regular physical activity not only aids in weight management but also helps in promoting proper digestion. Importantly, individuals suffering from acid reflux should avoid lying down immediately after meals, as this can exacerbate symptoms. By making these lifestyle changes, many find significant relief from their acid reflux symptoms.
2. Medications
When lifestyle modifications alone are insufficient, various medications can be prescribed to help manage acid reflux. Over-the-counter options such as antacids neutralize stomach acid and provide quick relief from heartburn. However, for chronic cases, physicians may recommend proton pump inhibitors (PPIs) or histamine-2 receptor antagonists (H2 blockers). These medications work by reducing the amount of acid produced by the stomach, thereby alleviating symptoms and preventing damage to the esophagus lining.
It is crucial to consult a healthcare provider before starting any medication, as prolonged use of certain options can lead to side effects or complications. For instance, long-term use of PPIs has been associated with an increased risk of certain infections and nutrient deficiencies. Therefore, a tailored approach based on individual needs and medical history is essential when considering medication for acid reflux.
3. Dietary Changes
Dietary modifications are a cornerstone of effective acid reflux diagnosis and treatment. The foods we consume directly influence the occurrence and severity of reflux symptoms. A diet high in fiber, vegetables, and lean proteins can support digestive health, while processed foods, high-fat items, and acidic foods are best avoided. Keeping a food diary can assist in identifying personal trigger foods, allowing individuals to make informed dietary choices.
Incorporating alkaline foods, such as bananas and melons, may also help neutralize stomach acid and provide relief. Additionally, staying hydrated by drinking plenty of water throughout the day can help dilute stomach acid and promote proper digestion. For those who enjoy cooking, experimenting with herbs and spices that are gentle on the stomach can make meals enjoyable without triggering reflux symptoms. Ultimately, a well-balanced diet tailored to individual needs is vital for managing acid reflux effectively.
4. Alternative Therapies
In recent years, many individuals have sought alternative therapies to complement traditional treatments for acid reflux. Practices such as acupuncture, yoga, and mindfulness meditation have gained popularity for their potential to reduce stress and promote relaxation. Stress is often a contributing factor to digestive issues, and finding effective ways to manage it can have a positive impact on symptoms.
Acupuncture, in particular, has shown promise in alleviating various digestive disorders, including acid reflux. By targeting specific points in the body, this ancient practice aims to restore balance and promote healing. Similarly, yoga can help improve digestion and reduce stress through gentle movement and breath control. While research on the efficacy of these alternative therapies is still evolving, many individuals report positive experiences and symptom relief through their incorporation into a comprehensive treatment plan.
5. Surgical Options
For those with severe acid reflux that does not respond to lifestyle changes or medications, surgical options may be considered. Procedures such as fundoplication involve wrapping the top of the stomach around the esophagus to prevent acid from backing up. While surgery is typically viewed as a last resort, it can provide long-term relief for individuals suffering from chronic reflux and its complications.
Before pursuing surgical intervention, a thorough evaluation by a healthcare professional is essential. This assessment will help determine the most appropriate course of action based on the severity of the condition, the presence of complications, and the overall health of the individual. While surgery can offer significant benefits, it is important to understand the risks involved and to have realistic expectations about the outcomes.
Conclusion
Navigating an acid reflux diagnosis and treatment can be overwhelming, but understanding the various options available empowers individuals to take control of their health. From lifestyle modifications and dietary changes to medications and alternative therapies, a range of strategies can help manage symptoms effectively. For those considering surgical options, consulting with a healthcare professional is crucial to ensure the best possible outcome.
At EIR DOC, we are committed to providing comprehensive care and support for individuals facing acid reflux. Our team of experts is dedicated to helping you find the most suitable treatment options tailored to your unique needs. Reach out to us today to explore how we can assist you on your journey toward better digestive health.
#anti acid reflux medication#medication for acid reflux in adults#acid reflux relief medicine#acid reflux diagnosis and treatment#prescription steroid cream for eczema online
0 notes
Text
Understanding Gastroesophageal Reflux Disease (GERD)

Gastroesophageal reflux disease (GERD) is a chronic condition where stomach acid frequently flows back into the esophagus, causing irritation and discomfort. While occasional acid reflux is common, GERD is diagnosed when it occurs regularly and disrupts daily life. Left untreated, GERD can lead to serious complications, including esophageal damage and other digestive disorders.
Causes of GERD
GERD occurs due to a malfunctioning lower esophageal sphincter (LES), the muscle at the end of the esophagus that closes to prevent stomach contents from flowing back. When the LES is weak or relaxes inappropriately, stomach acid can escape into the esophagus.
Several factors can contribute to GERD, including:
Diet: Consuming spicy, fatty, or acidic foods, along with caffeine and alcohol, can trigger reflux.
Obesity: Excess weight puts pressure on the abdomen, increasing the likelihood of acid reflux.
Smoking: Weakens the LES and increases acid production.
Pregnancy: Hormonal changes and pressure on the stomach can cause reflux.
Hiatal Hernia: A condition where part of the stomach pushes into the chest cavity, affecting the LES function.
Symptoms of GERD
Common symptoms of GERD include:
Heartburn: A burning sensation in the chest or throat, often after eating or lying down.
Regurgitation: A sour or bitter taste from stomach acid in the throat or mouth.
Difficulty Swallowing: Caused by narrowing or inflammation of the esophagus.
Chronic Cough or Sore Throat: Due to irritation from acid.
Chest Pain: Often mistaken for heart-related issues, it can occur with severe GERD.
If you experience these symptoms frequently, seeking care at a trusted stomach specialist hospital in Lakhanpur can provide a proper diagnosis and effective treatment.
Diagnosis
Diagnosing GERD typically involves:
Medical History and Physical Exam: Reviewing symptoms and lifestyle factors.
Endoscopy: A thin tube with a camera is used to inspect the esophagus and stomach for damage.
pH Monitoring: Measuring acid levels in the esophagus over 24 hours.
Manometry: Testing the strength and function of the LES and esophagus muscles.
Treatment Options
Treatment for GERD aims to alleviate symptoms, heal esophageal damage, and prevent complications. Common approaches include:
Lifestyle Changes:
Eat smaller meals and avoid trigger foods.
Maintain a healthy weight.
Avoid lying down immediately after eating.
Elevate the head of the bed while sleeping.
Medications:
Antacids: Neutralize stomach acid for immediate relief.
H2 Receptor Blockers: Reduce acid production.
Proton Pump Inhibitors (PPIs): Provide long-term relief by blocking acid production.
Surgery: For severe cases, procedures like fundoplication may be necessary to strengthen the LES. A leading stomach specialist hospital in Lakhanpur offers advanced surgical options for GERD management.
Complications of GERD
If untreated, GERD can lead to:
Esophagitis: Inflammation of the esophagus.
Strictures: Narrowing of the esophagus due to scar tissue.
Barrett’s Esophagus: A precancerous condition caused by long-term acid damage.
Esophageal Cancer: A rare but serious outcome in chronic cases.
Why Choose a Stomach Specialist Hospital?
Seeking care at a specialized stomach specialist hospital in Lakhanpur ensures access to experienced gastroenterologists and state-of-the-art diagnostic tools. These hospitals provide tailored treatment plans for GERD, addressing individual needs and promoting long-term digestive health.
Conclusion
GERD is a manageable condition when diagnosed and treated early. By understanding its causes, symptoms, and treatment options, you can take proactive steps toward relief and prevention. Consulting a reputable stomach specialist hospital in Lakhanpur ensures you receive expert care, enabling you to lead a healthier and more comfortable life free from the discomfort of GERD.
0 notes
Text
Peptic Ulcer Disease: Causes, Treatment, and How to Prevent It
Peptic ulcer disease (PUD) is a common gastrointestinal condition that affects millions of people worldwide. This condition involves painful sores or ulcers that develop in the lining of the stomach, lower esophagus, or the upper part of the small intestine. These ulcers can disrupt daily life, causing discomfort and complications if left untreated. At Gastro, Liver & Endoscopy Center, under the expert guidance of Dr. Manish Kumar Gupta, we aim to provide advanced care and treatment for peptic ulcer disease. Recognized as one of the Best Gastro Specialists in Ghaziabad, Dr. Gupta has extensive experience in diagnosing and treating a range of gastrointestinal disorders.

Understanding Peptic Ulcer Disease:
Peptic ulcers can be broadly classified into two categories based on their location:
Gastric Ulcers: These occur in the stomach lining.
Duodenal Ulcers: These develop in the upper part of the small intestine, called the duodenum.
While the symptoms and treatment of both types are similar, understanding the underlying causes is essential for proper diagnosis and management.
Causes of Peptic Ulcer Disease:
Peptic ulcers form when the balance between stomach acid and the protective mucus lining of the gastrointestinal tract is disrupted. This can occur due to:
Helicobacter Pylori Infection: The most common cause of peptic ulcers is an infection with Helicobacter pylori (H. pylori) bacteria. This bacteria weakens the stomach’s protective lining, allowing acid to irritate the underlying tissues.
Excessive Use of NSAIDs: Nonsteroidal anti-inflammatory drugs (NSAIDs) such as ibuprofen, aspirin, and naproxen can damage the stomach lining when used excessively or over a long period.
Stress and Lifestyle Factors: While stress and spicy foods do not directly cause ulcers, they can exacerbate symptoms. Smoking and excessive alcohol consumption can also increase the risk of developing ulcers.
Other Medical Conditions: Conditions like Zollinger-Ellison syndrome, which leads to excessive acid production, can also cause peptic ulcers.
Symptoms of Peptic Ulcer Disease:
Common symptoms of peptic ulcers include:
A burning sensation or pain in the abdomen, particularly between meals or at night.
Bloating and feeling full quickly.
Nausea or vomiting.
Dark, tarry stools, which may indicate bleeding.
If you experience any of these symptoms, it’s important to consult a specialist. At Gastro, Liver & Endoscopy Center, Dr. Manish Kumar Gupta and his team use state-of-the-art diagnostic tools to pinpoint the cause and severity of your condition.
Treatment Options for Peptic Ulcer Disease:
When it comes to treating peptic ulcers, a personalized approach is crucial. Recognized among the Top 10 Gastroenterologists in Ghaziabad, Dr. Gupta provides comprehensive care to help patients find relief.
Medications:
Antibiotics: To eradicate H. pylori infection, a combination of antibiotics is prescribed.
Proton Pump Inhibitors (PPIs): These medications reduce acid production and promote healing.
H2-Receptor Blockers: These also decrease stomach acid and alleviate symptoms.
Antacids: For immediate relief, antacids neutralize stomach acid.
Lifestyle Modifications: Dietary adjustments, quitting smoking, and reducing alcohol intake can improve symptoms significantly.
Endoscopic Procedures: In severe cases, endoscopy may be used to treat bleeding ulcers or to remove damaged tissues. Dr. Gupta specializes in advanced endoscopic techniques, ensuring minimal discomfort and faster recovery.
Surgery: Although rare, surgery might be necessary for complications such as perforation, obstruction, or severe bleeding.
Preventing Peptic Ulcer Disease:
While peptic ulcers can be effectively treated, prevention is always better than cure. Here are some tips to reduce your risk:
Limit NSAID Use: If you frequently use NSAIDs, consider alternatives or consult your doctor for protective medications.
Adopt a Healthy Diet: Eating a balanced diet rich in fruits, vegetables, and whole grains can strengthen your stomach lining. Avoid excessive spicy or acidic foods if they worsen your symptoms.
Quit Smoking and Limit Alcohol: Smoking and alcohol weaken the stomach’s natural defenses, making you more susceptible to ulcers.
Manage Stress: Practice stress-reducing activities like yoga, meditation, or regular exercise to improve overall gastrointestinal health.
Hygiene Practices: Since H. pylori can be transmitted through contaminated food or water, maintaining good hygiene is essential. Wash your hands frequently and ensure that your food and water are safe.
Why Choose Gastro, Liver & Endoscopy Center?:
If you’re searching for the Best Doctor for Gastroenterology in Ghaziabad, Dr. Manish Kumar Gupta at Gastro, Liver & Endoscopy Center is the trusted choice. With years of experience and a patient-centric approach, Dr. Gupta ensures that each patient receives personalized care. Here’s why our center stands out:
Expertise in advanced diagnostic tools like endoscopy and colonoscopy.
Comprehensive treatment plans tailored to individual needs.
Compassionate and professional staff dedicated to patient well-being.
Take the First Step Towards Healing:
Peptic ulcer disease can be distressing, but with timely diagnosis and treatment, it can be managed effectively. If you’re experiencing persistent abdominal pain, don’t ignore the symptoms. Visit the Gastro, Liver & Endoscopy Center to consult Dr. Manish Kumar Gupta, one of the Top 10 Gastroenterologists in Ghaziabad.
At our center, we’re committed to restoring your digestive health and improving your quality of life. Book an appointment today to start your journey toward a healthier tomorrow.
For appointments, call us at +91-9560720171 or visit our clinic at Plot No. - 100, Shakti Khand 2, Indirapuram, Ghaziabad. Let the Best Gastro Specialist in Ghaziabad take care of your gastrointestinal health.
#Best Gastroenterologist in Noida#Best Gastroenterologist in Noida Extension#Best Endoscopy Clinic in Ghaziabad#Best Endoscopy Centre in Ghaziabad#Best Endoscopy Centre in Indirapuram#Best Colonoscopy Centre in Indirapuram#Best Colonoscopy Centre in Ghaziabad#Best Endoscopy Centre in Noida#Best Endoscopy Centre in Delhi#Best Colonoscopy Centre in Noida#Best Colonoscopy Centre in Delhi
0 notes
Text
Trào ngược dạ dày gây mệt mỏi: Nguyên nhân, triệu chứng và cách chữa
Hiện tượng trào ngược dạ dày sẽ gây ảnh hưởng không hề nhỏ nếu người bệnh cảm thấy mệt mỏi, khó chịu kéo dài trong nhiều ngày. Không những vậy, đây cũng có thể là dấu hiệu cho thấy bệnh đã dần trở nên nguy hiểm hơn, gây rủi ro cho sức khỏe và thậm chí có thể ung thư dạ dày.
Trào ngược dạ dày gây mệt mỏi là gì?
Trào ngược dạ dày, hay còn gọi là trào ngược dạ dày thực quản (GERD), là tình trạng axit từ dạ dày trào ngược lên thực quản. Bệnh không chỉ gây ra các triệu chứng như ợ nóng, ợ chua mà còn dẫn đến tình trạng mệt mỏi kéo dài, ảnh hưởng nghiêm trọng đến chất lượng cuộc sống.

Nguyên nhân trào ngược dạ dày gây mệt mỏi
Suy giảm chất lượng giấc ngủ: Trào ngược dạ dày thường xảy ra vào ban đêm, gây khó chịu và làm gián đoạn giấc ngủ.
Thiếu hụt dinh dưỡng: Hệ tiêu hóa bị tổn thương khiến cơ thể khó hấp thụ các dưỡng chất, dẫn đến tình trạng suy nhược.
Stress và áp lực tâm lý: Trào ngược kéo dài làm gia tăng căng thẳng, từ đó khiến cơ thể mệt mỏi hơn.
Tác dụng phụ của thuốc: Một số loại thuốc điều trị dạ dày có thể gây buồn ngủ hoặc làm cơ thể thiếu năng lượng.
Triệu chứng trào ngược dạ dày gây mệt mỏi
Ợ nóng, ợ chua, cảm giác nóng rát ở vùng thượng vị.
Đau tức ngực hoặc khó nuốt.
Hơi thở hôi, cảm giác nghẹn cổ họng.
Mệt mỏi, uể oải, thiếu năng lượng dù ngủ đủ giấc.
Đau đầu, chóng mặt hoặc suy giảm khả năng tập trung.
Trào ngược dạ dày gây mệt mỏi nguy hiểm thế nào?
Nếu không được điều trị kịp thời, tình trạng này có thể dẫn đến các biến chứng nghiêm trọng như:
Viêm loét thực quản.
Hẹp thực quản do sẹo.
Barrett thực quản, làm tăng nguy cơ ung thư.
Cách điều trị trào ngược dạ dày gây mệt mỏi
1. Thay đổi lối sống
Chế độ ăn uống lành mạnh: Tránh các thực phẩm kích thích như đồ chiên rán, cay nóng, cà phê, rượu bia. Ăn chậm, nhai kỹ và chia nhỏ bữa ăn.
Hạn chế căng thẳng: Tập yoga, thiền định hoặc các bài tập thư giãn giúp giảm stress.
Ngủ đúng tư thế: Nâng cao phần đầu khi ngủ để giảm nguy cơ axit trào ngược.
2. Sử dụng thuốc
Các loại thuốc giảm axit như antacid, H2-receptor blockers hoặc thuốc ức chế bơm proton (PPI) thường được kê đơn.
Lưu ý: Chỉ sử dụng thuốc theo hướng dẫn của bác sĩ để tránh tác dụng phụ.
3. Điều trị chuyên sâu
Nếu các triệu chứng không thuyên giảm, người bệnh cần khám và điều trị tại các cơ sở y tế chuyên khoa. Một số trường hợp có thể cần phẫu thuật.
Phòng ngừa trào ngược dạ dày gây mệt mỏi
Duy trì cân nặng hợp lý để giảm áp lực lên dạ dày.
Không nằm ngay sau khi ăn, nên chờ ít nhất 2-3 giờ.
Uống đủ nước, bổ sung vitamin và khoáng chất cần thiết.
Khám sức khỏe định kỳ để phát hiện và điều trị bệnh sớm.
Trào ngược dạ dày gây mệt mỏi không chỉ ảnh hưởng đến hệ tiêu hóa mà còn tác động tiêu cực đến toàn bộ cơ thể. Hiểu rõ nguyên nhân, triệu chứng và các biện pháp điều trị sẽ giúp bạn kiểm soát bệnh tốt hơn, từ đó cải thiện chất lượng cuộc sống. Nếu tình trạng mệt mỏi kéo dài hoặc triệu chứng trở nên nghiêm trọng, hãy đến gặp bác sĩ ngay để được tư vấn.
Bài viết chi tiết: https://vienyduocdantoc.com/kien-thuc/trao-nguoc-da-day-gay-met-moi
Thông tin liên hệ Viện Y Dược Cổ Truyền Dân Tộc Tradimec
Website: https://vienyduocdantoc.com/
Địa chỉ: Biệt thự B31, KĐT Trung Hòa Nhân Chính, P. Nhân Chính, Q. Thanh Xuân, TP Hà Nội.
SĐT: (024) 7109 6699
Email: [email protected]
#vienyduocdantoc #vienyduoccotruyendantoc #tradimec
Tham khảo thêm các bài viết liên quan:
https://vienyduocdantoc.org.vn/benh-ly/trao-nguoc-da-day
https://vienyduocdantoc.org.vn/thuoc-chua/trao-nguoc-da-day
https://vienyduocdantoc.org.vn/an-uong/trao-nguoc-da-day-nen-an-gi
https://vienyduocdantoc.org.vn/cach-chua/trao-nguoc-da-day
0 notes
Text
Hiatal Hernia: Symptoms, Types, Causes, Treatment, and Prevention — Dr. Aniket Zarkar

Hiatal hernia is a common digestive condition where the upper part of the stomach pushes through the diaphragm into the chest cavity. Dr. Aniket Zarkar, a specialist in digestive health, provides expert insights into understanding hiatal hernias, their types, symptoms, and effective treatment options to manage the condition.
What Is a Hiatal Hernia?
A hiatal hernia occurs when a portion of the stomach moves upward through the diaphragm, the muscle that separates the chest from the abdomen. The diaphragm has a small opening (hiatus) through which the esophagus passes before connecting to the stomach. When part of the stomach pushes up through this opening, a hiatal hernia is formed.
Symptoms of a Hiatal Hernia
Many people with a hiatal hernia experience little to no symptoms, while others may develop significant discomfort. Common symptoms include:
Heartburn: acid reflux that causes a burning sensation in the chest or throat.
Regurgitation: acid or food coming back into the mouth or throat.
Difficulty swallowing: Especially when eating larger meals.
Chest pain: Often mistaken for heart-related issues.
Shortness of breath: Caused by pressure on the diaphragm.
Belching: Frequent belching or hiccups.
Types of Hiatal Hernia
There are two primary types of hiatal hernias:
Sliding Hiatal Hernia: The most common type, where the stomach and part of the esophagus slide in and out of the chest through the diaphragm. Sliding hernias often result in gastroesophageal reflux disease (GERD).
Paraesophageal Hiatal Hernia: Less common but more severe, as part of the stomach pushes next to the esophagus. This type can restrict blood flow, leading to a medical emergency if not treated promptly.
Causes of Hiatal Hernia
Several factors can contribute to the development of a hiatal hernia, including:
Age: As we age, the muscles supporting the diaphragm weaken, increasing the risk of hernias.
Increased Pressure: Lifting heavy objects, coughing, vomiting, or physical strain can put pressure on the diaphragm.
Obesity: Excess weight places added strain on the abdominal muscles.
Injury or Surgery: Trauma to the area or surgery near the diaphragm can lead to a hernia.
Genetic Factors: A congenital weakness or larger-than-normal hiatus can increase susceptibility.
Diagnosis of Hiatal Hernia
Dr. Aniket Zarkar may use various diagnostic tests to confirm the presence of a hernia:
Endoscopy: A flexible tube with a camera is used to view the esophagus and stomach.
Barium Swallow X-ray: This specialized X-ray visualizes the esophagus and stomach.
Esophageal Manometry: Measures the muscle contractions in the esophagus and the function of the lower esophageal sphincter.
Treatment Options for Hiatal Hernia
Treatment varies depending on the type and severity of the hernia.
1. Lifestyle Modifications
Eating smaller meals: Large meals can exacerbate symptoms.
Avoiding trigger foods: Spicy, acidic, and fatty foods can worsen reflux.
Weight management: Maintaining a healthy weight reduces abdominal pressure.
Elevation during sleep: Sleeping with the upper body elevated can help prevent acid reflux at night.
2. Medications
Antacids: Help neutralize stomach acid, providing temporary relief.
H2 Receptor Blockers and Proton Pump Inhibitors (PPIs): These reduce acid production and relieve symptoms of acid reflux.
3. Surgery
For those with severe or complicated hiatal hernias, surgical intervention may be necessary. Laparoscopic Nissen Fundoplication is the most common surgical procedure, where the stomach is repositioned and the esophageal sphincter is strengthened.
Preventing a Hiatal Hernia
While not all cases are preventable, certain measures can reduce the risk of developing a hiatal hernia:
Exercise regularly: Maintaining core strength and a healthy weight can reduce abdominal strain.
Avoid heavy lifting: Lifting heavy objects improperly can increase abdominal pressure.
Practice proper posture: Standing and sitting up straight can help reduce pressure on the abdomen.
Eat a balanced diet: High-fiber diets promote healthy digestion, reducing strain on the digestive tract.
Seeking Help with Dr. Aniket Zarkar
If you suspect a hiatal hernia or experience persistent digestive issues, consulting a specialist is essential. Dr. Aniket Zarkar provides advanced diagnosis and personalized treatment plans for patients dealing with hiatal hernias, helping them find relief from uncomfortable symptoms and regain quality of life.
#appendix treatment in hadapsar#gallbladder treatment in hadapsar#hernia treatment in hadapsar#piles specialist in hadapsar#fistula specialist in hadapsar
0 notes
Text
Mastering Receptor Blockers: A Comprehensive Guide | Nik Shah xAI
Receptor blockers, also known as antagonists, play a pivotal role in pharmacology by inhibiting the action of specific neurotransmitters or hormones at their respective receptors. This article explores the mechanisms, types, therapeutic uses, and future perspectives of receptor blockers.
Understanding Receptors and Blockers
Receptors are protein molecules located on cell membranes or within cells that bind to signaling molecules, such as hormones or neurotransmitters. When a signaling molecule attaches to its receptor, it initiates a cascade of biological responses. Receptor blockers interfere with this process by binding to the receptor without activating it, effectively blocking the action of the signaling molecule.
Mechanism of Action
Receptor blockers can work through various mechanisms, including:
Competitive Inhibition: The blocker competes with the natural ligand for binding to the receptor. This is common in many types of receptors, including adrenergic and histamine receptors.
Non-Competitive Inhibition: The blocker binds to a different site on the receptor or alters the receptor's conformation, preventing the natural ligand from exerting its effects.
Irreversible Blockade: Some blockers form a covalent bond with the receptor, leading to a long-lasting inhibition of receptor activity.
Types of Receptor Blockers
Receptor blockers can be categorized based on the receptors they target:
1. Adrenergic Blockers
These antagonists target adrenergic receptors (α and β), which are involved in the body’s response to stress. Common examples include:
Alpha Blockers: Used to treat hypertension and benign prostatic hyperplasia (BPH) by relaxing blood vessels.
Beta Blockers: Prescribed for heart conditions, anxiety, and migraine prevention by reducing heart rate and contractility.
2. Antihistamines
These blockers inhibit histamine receptors (H1 and H2), addressing allergic reactions and gastric acid secretion. H1 antagonists, such as diphenhydramine, are used for allergies, while H2 antagonists like ranitidine help reduce stomach acid.
3. Dopamine Antagonists
Dopamine receptor blockers are primarily used in treating psychiatric disorders. Medications like haloperidol and risperidone target dopamine receptors to manage symptoms of schizophrenia and bipolar disorder.
4. Opioid Antagonists
Drugs like naloxone and naltrexone block opioid receptors, reversing the effects of opioid overdose and aiding in addiction treatment by reducing cravings.
Therapeutic Applications
Receptor blockers have diverse therapeutic applications, including:
Cardiovascular Diseases: Beta blockers are vital in managing hypertension, heart failure, and arrhythmias.
Psychiatric Disorders: Dopamine antagonists are essential in treating schizophrenia, bipolar disorder, and severe depression.
Gastrointestinal Disorders: H2 blockers are effective for managing acid reflux and peptic ulcers.
Allergic Reactions: Antihistamines provide relief from allergic symptoms by blocking histamine action.
Future Perspectives
Research continues to expand the understanding and application of receptor blockers. Innovations include:
Targeted Therapies: Developing receptor blockers that selectively target specific receptor subtypes, minimizing side effects and enhancing efficacy.
Biologics: Investigating receptor blockers that utilize biological pathways, providing new avenues for treatment in complex diseases.
Personalized Medicine: Tailoring receptor blocker therapies based on genetic and phenotypic patient profiles to optimize treatment outcomes.
Conclusion
Mastering receptor blockers requires a deep understanding of their mechanisms, types, and therapeutic applications. As research evolves, the potential for innovative treatments will continue to grow, offering hope for more effective and personalized medical therapies. Whether addressing cardiovascular issues, psychiatric disorders, or allergies, receptor blockers remain a cornerstone of modern pharmacotherapy.
4o mini
#nikhilshah#nikplus#nikshah#architecture#artificial intelligence#books & libraries#business#chatgpt#claude#gemini#grok#xai
0 notes
Text
An Overview of the Reflux Esophagitis Pipeline Drugs Market
Gastroesophageal reflux disease (GERD), a chronic condition characterized by the upward flow of stomach acid into the esophagus, affects millions worldwide. The search for effective and safe treatments has fueled a robust pipeline of drugs targeting reflux esophagitis.

Buy the Full Report for More MoA Insights into the Gastroesophageal Reflux Disease Marketed Drugs, Download a Free Report Sample
Key Therapeutic Areas in the Pipeline
The pipeline for reflux esophagitis drugs focuses primarily on addressing the underlying causes of the disease, such as impaired lower esophageal sphincter (LES) function and increased acid production.
Proton Pump Inhibitors (PPIs): While PPIs are currently the mainstay of treatment, research is ongoing to develop novel PPIs with improved efficacy and safety profiles.
H2 Receptor Antagonists: Although second-line agents, there's continued interest in developing more potent and long-acting H2 blockers.
Gastric Motility Agents: Drugs targeting gastric motility disorders, which contribute to GERD, are under investigation.
Local Esophageal Therapies: Development of drugs with local action on the esophageal mucosa to heal inflammation and protect against acid damage.
Neuromodulators: Targeting neurotransmitters involved in esophageal function to address GERD symptoms.
Key Players and Their Pipeline
Several pharmaceutical companies are actively involved in the development of new treatments for reflux esophagitis. While established players like AstraZeneca, Pfizer, and Takeda have a strong presence, there's also a growing number of biotech companies focusing on this therapeutic area.
AstraZeneca: The company has a pipeline of drugs targeting different aspects of GERD, including acid suppression and mucosal protection.
Pfizer: With a strong portfolio of gastrointestinal drugs, Pfizer continues to invest in research and development for GERD.
Takeda: The acquisition of Shire has expanded Takeda's presence in the gastrointestinal disease area, including GERD.
Challenges and Opportunities
The development of new drugs for reflux esophagitis is a complex process. Key challenges include:
High Development Costs: The cost of clinical trials and regulatory hurdles can be substantial.
Competitive Landscape: The market is already crowded with existing treatment options, making it challenging for new drugs to gain market share.
Patient Heterogeneity: The diverse nature of GERD symptoms and patient populations makes it difficult to develop a one-size-fits-all treatment.
Despite these challenges, the pipeline for reflux esophagitis drugs holds significant promise. The potential to develop more effective and well-tolerated treatments could significantly improve the lives of millions of patients suffering from this condition.
0 notes
Text
What are different types of hernia and their effective treatments?

Hernias are classified based on their location and the cause. Here are some common types of hernias and their respective treatments:
1. Inguinal Hernia
Location: Groin area
Symptoms: Bulge in the groin, pain or discomfort, especially when bending over, coughing, or lifting
Treatment: Conservative Management: Watchful waiting for asymptomatic or minimally symptomatic hernias Surgical Repair: Open Hernia Repair: Involves a larger incision to place the protruding tissue back into the abdomen and strengthen the abdominal wall with stitches or synthetic mesh. Laparoscopic Repair: Minimally invasive surgery using small incisions, a camera, and specialized instruments to repair the hernia.
2. Femoral Hernia
Location: Upper thigh, near the groin
Symptoms: Bulge in the upper thigh, pain or discomfort, especially when straining or lifting
Treatment: Surgical Repair: Often recommended due to the risk of complications like strangulation. Open Surgery: A traditional approach with a single larger incision. Laparoscopic Surgery: A minimally invasive approach using smaller incisions.
3. Umbilical Hernia
Location: Near the belly button
Symptoms: Bulge near the navel, pain or discomfort
Treatment: Conservative Management: Watchful waiting in infants as many umbilical hernias close on their own. Surgical Repair: Recommended for adults or persistent hernias in children, using either open or laparoscopic techniques.
4. Hiatal Hernia
Location: Upper stomach pushing through the diaphragm
Symptoms: Heartburn, acid reflux, difficulty swallowing
Treatment: Medication: To manage symptoms (e.g., antacids, H2 receptor blockers, proton pump inhibitors) Surgery: For severe cases or complications, typically performed laparoscopically.
5. Incisional Hernia
Location: At the site of a previous surgical incision
Symptoms: Bulge near a previous surgical scar, pain, or discomfort
Treatment: Surgical Repair: Necessary for most cases, either via open surgery or laparoscopic techniques.
6. Epigastric Hernia
Location: Upper abdomen, between the navel and the lower part of the rib cage
Symptoms: Small bulge in the upper abdomen, pain or discomfort
Treatment: Surgical Repair: Often recommended to prevent complications, using either open or laparoscopic surgery.
7. Ventral Hernia
Location: Any part of the abdominal wall
Symptoms: Bulge in the abdominal area, pain, or discomfort
Treatment: Surgical Repair: Typically involves reinforcing the abdominal wall with mesh, can be performed via open or laparoscopic surgery.
Conclusion
Each type of hernia has its own set of symptoms and hernia treatment options. Surgical repair is a common and effective treatment for most hernias, especially if they cause pain or other symptoms, or have a risk of complications.
Consulting with a healthcare provider is essential to determine the best course of action for your specific condition.
#hernia surgery#hernia treatment#hernia specialist#herniatreatment#hernia doctor#hernia surgeon#herniarecovery
0 notes
Text
Medicine for Instant Relief from Acidity: Your Go-To Guide
Experiencing acidity can be incredibly uncomfortable and disruptive to your day. Whether it's a result of diet, stress, or other factors, finding a quick and effective solution is often a top priority. This guide will explore various medicines for instant relief from acidity, ensuring you can get back to feeling your best in no time.

Understanding Acidity
Before exploring into specific remedies, it's helpful to understand what causes acidity. Acidity occurs when there is an excess production of stomach acid, leading to symptoms like heartburn, indigestion, and discomfort. Common triggers include spicy foods, caffeine, alcohol, stress, and certain medications.
Medicines for Instant Relief from Acidity
1. Antacids
Antacids are the most common over-the-counter (OTC) medications for instant relief from acidity. They work by neutralizing stomach acid, providing quick relief from symptoms. Popular antacids include Tums, Rolaids, and Mylanta. These are ideal for occasional use but should not be relied upon for long-term management.
2. H2 Receptor Blockers
H2 receptor blockers, such as ranitidine (Zantac) and famotidine (Pepcid), reduce the amount of acid the stomach produces. They provide longer-lasting relief compared to antacids and are suitable for both immediate and preventative use. These medications can be found OTC or prescribed by a healthcare provider.
3. Proton Pump Inhibitors (PPIs)
PPIs, including omeprazole (Prilosec) and esomeprazole (Nexium), are highly effective for treating chronic acidity and gastroesophageal reflux disease (GERD). They work by blocking the enzyme responsible for acid production, offering longer relief. PPIs are typically taken once daily and are available both OTC and by prescription.
4. Alginate Drugs
Alginate drugs like Gaviscon create a protective barrier in the stomach, preventing acid from rising into the esophagus. This can provide instant relief from acidity and is particularly useful for individuals who experience reflux after meals.
Natural Remedies
While OTC and prescription medications are effective, some prefer natural remedies for instant relief from acidity. These include:
Ginger: Known for its anti-inflammatory properties, ginger can help soothe the stomach.
Aloe Vera Juice: This can reduce inflammation and provide a cooling effect.
Apple Cider Vinegar: Diluted in water, it may help balance stomach acid levels.
Baking Soda: A teaspoon in a glass of water can neutralize stomach acid.
When to See a Doctor
While occasional acidity is common, frequent or severe symptoms may indicate a more serious condition, such as GERD or an ulcer. If you experience symptoms more than twice a week or if OTC medications do not provide relief, it's important to consult a healthcare provider for a comprehensive evaluation and appropriate treatment plan.
Conclusion
Finding the right medicine for instant relief from acidity can significantly improve your quality of life. Whether you opt for antacids, H2 receptor blockers, PPIs, or natural remedies, there are numerous options available to suit your needs. Remember to monitor your symptoms and seek medical advice if necessary to ensure effective and safe treatment.
By understanding your options and making informed choices, you can effectively manage acidity and enjoy a more comfortable, symptom-free life.
1 note
·
View note
Text
5 Common Gastrointestinal Diseases and Their Symptoms, Treatments

The digestive system plays an important role in our overall health. When it is functioning well, we notice its presence, but when something goes wrong, the impact on our daily lives can be effective. Gastrointestinal diseases refer to any conditions that impact the digestive system, including the esophagus, stomach, intestines, liver, gallbladder, and pancreas. These diseases can range from mild discomfort to serious health complications. Factors like age, genetics, lifestyle choices, and diet can increase the risk of developing these conditions. Here, we discuss five common gastrointestinal diseases, their symptoms, and the treatments available by a gastro surgeon Ahmedabad.
5 Common Gastrointestinal Diseases, Their Symptoms And Treatment with Gastro Surgeon Ahmedabad:
1. Gastroesophageal Reflux Disease (GERD)
GERD is a prevalent condition where stomach acid frequently flows back into the esophagus, irritating.
Symptoms:
Gastroesophageal Reflux Disease, commonly known as GERD, occurs when stomach acid frequently flows back into the tube connecting your mouth and stomach (esophagus). This backwash can irritate the lining of your esophagus. Common symptoms include heartburn, regurgitation of food or sour liquid, chest pain, difficulty swallowing, and a sensation of a lump in your throat.
Treatment:
Lifestyle changes are the first line of protection, including avoiding foods that trigger symptoms, eating smaller meals, not lying down after eating, and losing weight if overweight. Medications such as antacids, H2 receptor blockers, and proton pump inhibitors (PPIs) are commonly prescribed. In severe cases, surgery might be recommended by a gastro surgeon Ahmedabad, such as fundoplication, where the top of your stomach is sewn around the esophagus to tighten the sphincter.
2. Irritable Bowel Syndrome (IBS)
IBS is a common disorder affecting the large intestine, characterised by a combination of abdominal discomfort and altered bowel habits.
Symptoms:
Irritable Bowel Syndrome (IBS) is a common disorder affecting the large intestine. It is characterised by a group of symptoms, including cramping, abdominal pain, bloating, gas, diarrhea, and constipation. IBS is a chronic condition that requires long-term management.
Treatment:
Treatment of IBS focuses on relieving symptoms so that you can live as normally as possible. Mild signs and symptoms can often be controlled by managing stress and by making changes in diet and lifestyle. More severe symptoms can be managed with medication. For example, fiber supplements or laxatives may help with constipation, while anti-diarrheal medications can be used when diarrhea is the main issue. Anticholinergic medications can help relieve painful bowel spasms.
3. Celiac Disease:
Celiac disease is an autoimmune disorder where ingestion of gluten leads to damage in the small intestine.
Symptoms:
Celiac disease is an autoimmune disorder where the ingestion of gluten leads to damage in the small intestine. Over time, the body’s immune system reacts to gluten (a protein found in wheat, barley, and rye) by attacking the small intestine. This leads to symptoms such as diarrhea, bloating, gas, fatigue, weight loss, anemia, and even osteoporosis.
Treatment:
The only effective treatment for celiac disease is a strict, lifelong gluten-free diet. This involves avoiding all foods containing wheat, barley, and rye. A gastro surgeon Ahmedabad can guide managing the disease and monitor for any probable complications. Regular follow-ups and nutritional counselling are also recommended to ensure the patient is receiving adequate nutrition despite dietary restrictions.
4. Crohn’s Disease
IBD is an umbrella term that includes Crohn’s disease and ulcerative colitis, both of which involve chronic inflammation of the GI tract.
Symptoms:
Crohn’s disease is a type of inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal tract, from the mouth to the anus. The inflammation caused by Crohn’s can lead to a wide range of symptoms, including diarrhea, fever, fatigue, abdominal pain and cramping, blood in your stool, mouth sores, reduced appetite, and weight loss. The severity of symptoms can range from mild to severe and can develop slowly or come on suddenly without warning.
Treatment:
There is no cure for Crohn’s disease, but there are treatments that can help manage the symptoms. Anti-inflammatory drugs, immune system suppressors, antibiotics, and other medications can be used to reduce inflammation and manage symptoms. Nutritional supplements may also be necessary, as Crohn’s disease can affect the ability to absorb nutrients. In severe cases, surgery might be necessary to remove damaged portions of the digestive tract.
5. Gastroenteritis:
Gastroparesis is a condition where the stomach’s ability to empty its contents is delayed, causing various digestive symptoms.
Symptoms:
Gastroenteritis, often referred to as the stomach flu, is an inflammation of the stomach and intestines, usually caused by a viral or bacterial infection. Symptoms include watery diarrhea, abdominal cramps and pain, nausea, vomiting, occasional muscle aches or headaches, and a low-grade fever. Dehydration is a common complication, especially in children and older adults.
Treatment:
Most cases of gastroenteritis resolve on their own within a few days. The primary treatment is to prevent dehydration by drinking plenty of fluids. Oral rehydration solutions can be used to replace lost electrolytes. In more severe cases, hospitalisation may be required for intravenous fluids. Antiemetic and antidiarrheal medications can be used to manage symptoms, but antibiotics are only recommended by a gastro surgeon Ahmedabad if a bacterial infection is confirmed.
Conclusion
Gastrointestinal diseases can greatly impact a person’s quality of life. Early detection and treatment are crucial in managing symptoms and preventing complications. If you are experiencing symptoms related to these conditions, it is important to consult a gastro surgeon Ahmedabad for a careful evaluation and personalised treatment plan. Remember, with the right lifestyle changes and medical interventions, many of these conditions can be effectively managed, allowing you to lead a healthy and fulfilling life.
0 notes
Text
Managing Acid Reflux: A Look at the Best Relief Medicines
Acid reflux, also known as gastroesophageal reflux disease (GERD), is a common condition that affects millions of individuals worldwide. It occurs when stomach acid flows back into the esophagus, causing discomfort, heartburn, and other unpleasant symptoms. The management of acid reflux relief medicine often requires a comprehensive approach that combines lifestyle modifications with the use of effective medications. Understanding the various types of relief medicines available can empower those suffering from this condition to make informed choices that enhance their quality of life.

Understanding Acid Reflux and Its Symptoms
Before delving into the different types of medications for acid reflux, it is crucial to comprehend what this condition entails. Acid reflux occurs when the lower esophageal sphincter (LES), a muscle that separates the stomach from the esophagus, relaxes abnormally or weakens. This allows stomach acid to escape into the esophagus, leading to a variety of symptoms. Common indications include a burning sensation in the chest known as heartburn, regurgitation of sour or bitter-tasting acid, difficulty swallowing, and in some cases, a persistent cough or sore throat.
For many people, these symptoms can disrupt daily life, making it essential to seek effective relief options. While lifestyle changes such as dietary adjustments, weight management, and avoiding trigger foods play a significant role in managing acid reflux, the use of medications can provide additional support.
Antacids: Immediate Relief for Mild Symptoms
One of the most immediate forms of relief for acid reflux symptoms comes from antacids. These over-the-counter medications work by neutralizing stomach acid, providing quick comfort from heartburn and indigestion. Popular antacids include formulations containing ingredients such as magnesium hydroxide, aluminum hydroxide, and calcium carbonate. The appeal of antacids lies in their rapid action; many individuals find relief within minutes of ingestion.
However, while antacids can effectively alleviate mild symptoms, they do not address the underlying cause of acid reflux. Frequent use can lead to potential side effects, such as diarrhea or constipation, depending on the active ingredients. Therefore, while antacids can be a useful short-term solution, they should not be relied upon as a long-term remedy without consulting a healthcare professional.
H2 Blockers: Reducing Acid Production
For those experiencing more frequent or severe acid reflux symptoms, H2 blockers may offer a more effective solution. H2 blockers, or histamine-2 receptor antagonists, work by reducing the amount of acid produced by the stomach. Commonly prescribed H2 blockers include ranitidine, famotidine, and cimetidine.
The benefits of H2 blockers extend beyond immediate relief. By decreasing acid production, these medications can help prevent the occurrence of reflux episodes, providing a more sustained approach to managing symptoms. H2 blockers typically take longer to provide relief compared to antacids, often requiring several hours for their effects to be felt. However, they can be taken in advance of meals or at bedtime to prevent nighttime symptoms.
While generally well-tolerated, H2 blockers may cause side effects in some individuals, including headaches, dizziness, and gastrointestinal disturbances. Long-term use can also lead to tolerance, where the body becomes less responsive to the medication, necessitating higher doses for the same effect. Therefore, it is crucial to work closely with a healthcare provider to determine the appropriate use of H2 blockers in managing acid reflux.
Proton Pump Inhibitors (PPIs): Stronger Acid Control
For individuals with chronic acid reflux, proton pump inhibitors (PPIs) represent a powerful option for controlling stomach acid production. PPIs, such as omeprazole, esomeprazole, and lansoprazole, are particularly effective for those who do not find sufficient relief with antacids or H2 blockers. By blocking the proton pumps in the stomach lining, these medications significantly reduce acid secretion, providing longer-lasting relief.
PPIs are often recommended for individuals with more severe GERD symptoms or those experiencing complications from acid reflux, such as esophagitis or Barrett's esophagus. The relief offered by PPIs can last for up to 24 hours, making them suitable for once-daily dosing. However, it is essential to note that long-term use of PPIs has been associated with certain risks, including an increased likelihood of gastrointestinal infections, nutrient malabsorption, and potential kidney issues. Therefore, healthcare providers typically recommend using PPIs for the shortest duration necessary to manage symptoms effectively.
Lifestyle Modifications: Complementing Medication
While medications play a crucial role in managing acid reflux, they are most effective when combined with lifestyle modifications. Simple changes in daily habits can significantly reduce the frequency and severity of symptoms. For instance, maintaining a healthy weight is paramount, as excess weight can put pressure on the stomach, exacerbating reflux.
Dietary adjustments can also yield substantial benefits. Identifying and avoiding trigger foods—such as spicy dishes, citrus fruits, and high-fat meals—can help minimize symptoms. Additionally, adopting smaller, more frequent meals rather than large portions can aid digestion and reduce reflux episodes. It is also advisable to refrain from lying down or engaging in strenuous activities immediately after eating, as these actions can hinder the body's natural digestive processes.
Conclusion: A Holistic Approach to Managing Acid Reflux
In conclusion, effectively managing acid reflux requires a multifaceted approach that encompasses medication, lifestyle changes, and ongoing communication with healthcare providers. Understanding the different types of relief medicines—antacids for immediate relief, H2 blockers for moderate symptoms, and PPIs for severe cases—enables individuals to make informed choices in their treatment journey.
However, it is important to remember that no single solution fits all. Each person's experience with acid reflux is unique, and what works for one individual may not be suitable for another. Therefore, maintaining an open dialogue with a healthcare professional is crucial for tailoring a management plan that addresses specific needs and concerns. By embracing a comprehensive strategy that includes both medications and lifestyle modifications, individuals can regain control over their lives and enjoy a better quality of life free from the burdens of acid reflux.
1 note
·
View note
Text

Understanding and Managing Gastric Ulcers: Causes, Symptoms, and Management
Gastric ulcers, also known as stomach ulcers, are open sores that develop on the inner lining of the stomach. These ulcers can cause significant discomfort and may lead to serious complications if left untreated. Understanding the causes, recognizing the symptoms, and seeking appropriate treatment from the best gastroenterologist in Chennai, such as Dr. Kumargurubaran, are essential steps in managing this condition.
Causes of Gastric Ulcers
Gastric ulcers are primarily caused by an imbalance between digestive fluids in the stomach and duodenum. The most common factors contributing to this imbalance include:
Helicobacter pylori (H. pylori) Infection: This bacterium weakens the stomach's protective mucous lining, making it more susceptible to damage from stomach acid. Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): Regular use of NSAIDs, such as ibuprofen and aspirin, can irritate the stomach lining and lead to ulcer formation. Excessive Acid Production: Conditions such as Zollinger-Ellison syndrome can cause the stomach to produce excessive amounts of acid, leading to ulcer development. Smoking and Alcohol: Both smoking and excessive alcohol consumption can irritate and erode the stomach lining. Stress and Diet: While not direct causes, stress and a poor diet can exacerbate the symptoms of gastric ulcers. Symptoms of Gastric Ulcers
The symptoms of gastric ulcers can vary in intensity and may include:
Burning Stomach Pain: The most common symptom, often occurring between meals or at night. Bloating and Belching: Feeling full quickly and frequent burping. Nausea and Vomiting: Sensation of nausea, sometimes leading to vomiting. Weight Loss: Unintentional weight loss and loss of appetite. Bloody Stools or Vomit: Indicating a more severe ulcer that requires immediate medical attention. If you experience any of these symptoms, it's crucial to consult a gastro specialist in Chennai for accurate diagnosis and treatment.
Managing Gastric Ulcers
Effective management of gastric ulcers involves a combination of medical treatment and lifestyle modifications. Here are some key strategies:
Medications: Antibiotics: To eradicate H. pylori infection. Proton Pump Inhibitors (PPIs): Reduce stomach acid production. H2-Receptor Blockers: Decrease acid production. Antacids: Neutralize existing stomach acid. Dietary Changes: Avoid spicy, acidic, and fatty foods that can irritate the stomach lining. Eat smaller, more frequent meals to avoid overloading the stomach. Lifestyle Modifications: Quit smoking and limit alcohol consumption. Manage stress through relaxation techniques and regular exercise. Regular Monitoring: Schedule follow-up visits with the best gastro doctor in Chennai to monitor progress and adjust treatment as needed. Surgical Intervention: In severe cases, surgery may be necessary. The best gastro surgeon in Chennai, such as Dr. Kumargurubaran, can perform procedures to remove ulcers or reduce acid production. Conclusion
Understanding the causes and symptoms of gastric ulcers is the first step in effective management. By consulting with a top gastroenterologist in Chennai like Dr. Kumargurubaran, you can receive comprehensive care tailored to your needs. With appropriate medical treatment, dietary adjustments, and lifestyle changes, you can manage gastric ulcers effectively and improve your overall gastrointestinal health.
DrKumaragurubaran Best Gastroenterologist Surgeon in Chennai/Hernia/Gallbladder/Fistula/Laparoscopic Surgeon.
Address: Billroth Hospitals, B, block 43, Lakshmi Talkies Rd, Shenoy Nagar, Chennai, Tamil Nadu 600030
#best gastro doctor chennai#best gastroenterologist in chennai#best gastro surgeon in chennai#gastro specialist in chennai#best laparoscopic surgeon chennai#best gastroenterologist chennai#best gastro surgeon chennai#gastro specialist chennai
0 notes