#''we are questioning the very foundation of psychiatry which uses mental illness; which is often just behavior that is judged strange
Explore tagged Tumblr posts
Text
forgive any incomprehensibility but the notion that the world can be cleanly split between the two immutable categories of 'the neurotypical' and 'the neurodiverse' ignores the reality that any person can at any point for any reason be arbitrarily 'diagnosed' by a 'professional' and shuttled between categories with no regard for the notions of 'accurate traits' or 'specific symptoms'. nice dichotomy what lies outside of it? you understand me?
#N posts stuff#i'm reading some old issues of 'Phoenix Rising' and a line in one of the articles really caught me#''we are questioning the very foundation of psychiatry which uses mental illness; which is often just behavior that is judged strange#by some usually conventional middle-class-standard of morality''#also thinking about that post i reblogged yesterday claiming that 'posture sway' is a Symptom of adhd like.#Embracing the pathologizing of average behaviors VS the like. weaponizing of diagnoses against 'undesirables'#idk am i making sense? lol#like people talk about this re: disability - the notion that anyone can become disabled at any time but that's usually in the context#of like. 'anyone is one bad accident away from being disabled' but Neurodiversity in particular does not even require that much#another Phoenix Rising tells the story of a woman who like. got a little sick at work and diagnosed as 'stress' and prescribed a#heavy tranquilizer that caused side effects no one had told her about; she got confused at her appointment and her subsequent#panic got her involuntarily committed as psychotic where they upped the medications and gave her ECT until the combo#caused so much brain damage that she seized and died. bc she threw up at work one day. the categories are not immutable and#the people who define them have agendas. who benefits from buying into this dichotomy? you understand what i'm saying?#anti psychiatry
49 notes
·
View notes
Note
Hello! If you don't mind me asking what do you mean with "anti-psychiatry" is it psychiatry itself or how mentally ill people are often treated in it, or something else? As someone who's mentally ill and loves psychology and one day want to become something in it, I want to know if there's things I should avoid.
I mean mostly that there are a few ideas that are foundational to psychiatry, which is specifically a discipline dedicated to easing emotional distress through medicinal intervention. These foundations are:
1. It is possible to group symptoms into syndromes and disorders, which can then be discussed coherently, such that people who "have" depression or any other disorder can be discussed as a group. This is a falsehood in my opinion. There are many reasons a person may experience significant emotional distress- I know almost no people who've been diagnosed with a mental illness whose life experiences, especially as children, are not sufficient to explain why they have problems with socialization, or emotional regulation, or self soothing, or general engagement with the outside world.
2. One of the primary reasons for emotional distress that can be diagnosed as a disorder, is a chemical problem in the brain. Most psychiatrists now know that there is not and has never been sufficient science to support the idea that, say, depression is a result of a biochemical problem in the brain. The evidence straight up is not there. Yet patients overwhelmingly believe this to be the case and psychiatrists are happy to let them believe that medication will "fix" their problem, which they posit is not a set of circumstances or unresolved emotional work but a disease. At best this is widespread medical malpractice, and it includes a lot of intentional deception by psychiarists.
3. In a very large percentage of cases, medication is one of the best treatment options on the table. Increasingly, this means longterm prescription of drugs whose long term effects are simply not known. There is an increasingly large body of evidence suggesting that longterm use of certain kinds of drugs actually increases the likelihood of continued need for those drugs by essentially hobbling whatever mechanisms the brain uses to stay stable.
I think it's very clear that some people do benefit from the use of certain psychiatric drugs- I took psychiatric medication myself for about a year and a half and only stopped because I had no medical insurance and then stayed off because I used my time off medication to work on my emotional problems- but psychiatry as a science simply has a long way to go to develop itself as a reliable and trustworthy science in my opinion, and certainly I think when we have gotten to a point where the NUMBER of people who are currently on antidepresants or antianxiety medications is so massive, I think we should be questioning not just how widespread that use is, but the very bases of psychiatry as a science.
59 notes
·
View notes
Text
Closer To The End (part III)
I contend that human beings are not suited for the world we've fashioned for ourselves. Cases of anxiety and depression are practically ubiquitous, and suicide in all age groups is once again on the rise. Some will suffer mental afflictions that last years -- perhaps even for a lifetime. This is the third and final part of my story.

~By Billy Goate~
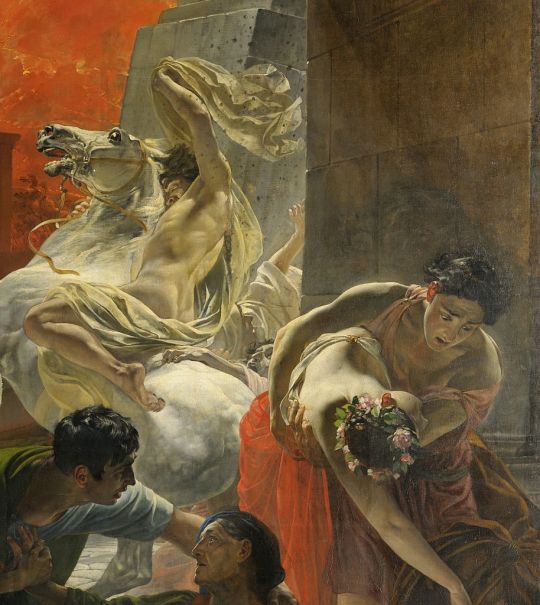
Cover art by Ruso Tsig additional art by Karl Briullov
I'm so tired of hearing that I'm wrong Everyone laughs at me, why me? I'm so tired of being pushed around I feel like I've been betrayed
youtube
We take each other's love, forget to give back Isn't it a pity, how we break each other's hearts I know we're only human and not to blame But who the hell are you to cause so much pain Why...
MEDICATION

My parents have been anti-establishment for as long as I can remember. In the climate of the 1980s, the institutions of the day were being called seriously into question. One of them was the authoritarian nature of public education (there's a reason why Pink Floyd's "Another Brick in the Wall" resonated so strongly with people). It's no surprise that my family got caught up in the first wave of the homeschooling movement. Other areas of modern life began to be called into question, as well, taking the family down a dark, windy road that led into conspiracy culture, extreme libertarianism, and religious dogmatism.
This distrust of the "experts" put us at odds with the medical establishment, too. "Doctors only know how to do two things," mom would often proclaim loudly in one of her famous rants, "cut you open or prescribe you pills." Natural medicine held the keys to recovery from all ills, be it cancer or the common cold. "All those chemicals aren’t good for your body," she insisted. "God put everything we need for healing in the ground." I’m not here to knock naturopathy (I was an ardent follower of this way of life for years) nor my mother for her convictions, but there are some things that can’t be cured by Saint John's Wort and herbal tea -- major depression being one of them.
At one point, my anxiety, melancholy, and a generalized feeling of social isolation reached such a heightened state I turned to hypnotism, enamored by an obscure radio program hosted by Roy Masters and his Foundation for Human Understanding. I was too young to understand the significance of most of the bullshit he was spewing, but it was the comprehensive approach to life that appealed to me. I wanted answers -- all of them. About the only thing I got out of it, though, was learning how to make my own arm go numb through self-hypnosis.
Later, I'd get caught up in a movement of Biblical counseling that rejected psychiatry altogether. "Christ has given us all things we need for life and godliness," says the holy writ, ergo we need none other than Jesus to cure our mental ills. Furthermore, the thesis said, since "God has not given us a spirit of fear" it must mean that the root of depression and anxiety is ultimately sin against God. The answer? Confess your sins and walk by faith, not by sight. In short, pray the sadness away. All of this had limited effectiveness in coping with the claustrophobic cloud of melancholy that was constantly with me.
Cough & Windhand: Reflection of the Negative by Windhand
The stigma of psychiatry and modern medicine kept me from treating my depression for damn near a decade. Somewhere in my late twenties, after a prolonged and particularly dark depressive spell, I decided to talk to my medical doctor about antidepressants. He started me on the industry standard, the well-known and well-marketed Prozac, which became a household name in the '90s. I took the first dose at bedtime and when I woke up, I was seriously hating the daylight. Feeling extraordinarily fatigued, all I wanted to do was sleep. I called in a rare sick day from work. The next day I was feeling groggy, but well enough to return. Giving it the good ol' college try, I took Prozac for several weeks as directed, but the side-effects just weren't worth it for me. That’s when I was referred to my first psychiatrist.
It was a weird feeling sitting in the waiting room for my appointment. I felt like I’d joined the ranks of the fragile, broken, and confused, perhaps even the insane. It was hard for me to see myself sharing anything in common with the others that shared the tiny lobby. The psychiatrist who greeted me looked like a regular chucklehead -- you know, one of those sidekicks from a sitcom that's not coming to me now. (It just came to me: Glen from the Tom Green Show.) A paunchy man in his 30s with wavy dirty blonde hair parted to the side donning wire-rimmed glasses, the shrink pulled out a notebook and started asking me about my background, while he busily took notes. Turned out, the man was very methodical in his approach. Over the course of the year, we cycled through all kinds of drugs -- Paxil, Effexor, Wellbutrin, Lexapro, Zoloft, and a lot of other names I'm not remembering, before finally settling on Cymbalta.
Certainly, this was something I didn't want to share with my coworkers, much less mom and dad. The first time I told my brother I was taking antidepressants, he was outraged. “You don’t need that stuff in your body. You don’t need pills to feel good.” I don’t know what it is about antidepressant medication that offends people so badly, but some people feel it is their personal mission in life to get you off of them. Why all the evangelical fervor? Are they secretly afraid they are "nuts," too? It’s not like I’m trying to get everyone else to take my medication, but suddenly these people, well-meaning or not, are trying to get you off of your meds.
I’ve seen YouTube videos from a guy claiming that God has cured him of his bipolar disorder and he flushed all his pills down the toilet (bad idea, by the way). Then a month later, he comes back online crying uncontrollably, talking about how he feels like God is testing him and asking viewers to pray to stop Satan’s onslaught. Moral of the story: It's dangerous to let people's religious opinions and untested hunches drive the agenda for our mental health.
I'm very reluctant these days to talk to anyone about my depression, because of all the rush to judgement involved. Ironically, it's this breakdown of community that I believe is at the heart of much of our mental health issues as a society. Look at the comments on any confessional video addressing burnout, depression, or anxiety and you'll find everyone is suddenly an expert who knows so well the precise and perfect solution to your problems. Well-meaning or not, it's incredibly annoying and I'd rather not have trouble with it. Hell, it took me two years to finish this article.

Depressed people are often viewed with the same cynical dismissiveness ascribed to angsty hormonal teens. "It's just a phase, you'll get through it," you're told with the reassuring wave of a hand. Besides, they remind you, "Happiness is a choice!" Because they are feeling chipper today, they have little patience for you dampening their mood. Others call you edgy when you say the pressures of life are so great that you feel like just turning off the lights on all of it. Still others will view you as selfish for leaving the family reunion early (or not wanting to participate in holidays at all). When you spend the whole weekend in bed sleeping, they'll accuse you of being indulgent, not realizing sleep gives you a respite from the hurt, guilt, and regret of painful memories or the misery of an unstable home life. Or the well-meaning "It Gets Better!" It doesn't always get better as life moves on.
Then there are those who try to talk you off your meds, entirely (cue: the ridiculously overwrought Facebook posts). We've all been privy to those conversations that strike a conspiratorial tone about how it was really the pharmaceutical companies that led to Chris Cornell's death. "You should just get off the stuff," they argue -- be it from noble intentions or just pride from clinging to an opinion they've stubbornly invested in.
Then there are those who are convinced that since Jesus (or Buddha, Allah Oprah, Jordan Peterson or juicing) gave them an escape from their depression, certainly it is the universal cure for all that ails you. Understand that I was a committed Christian for decades. I know what it is like to feel spiritually serene and I value many of the things the church gave me as a young adult, namely the fellowship, tolerance, and love. I know the feeling of peace that comes from believing in someone who reigns over the chaos and cares about your every need -- an ultimate being who will make sense of the nonsense one day.
I don't wish to diminish anyone's faith or diminish your personal experiences. The fact is, however, that major depression is as much a physical illness as cancer is. Certainly, there are transitional feelings of unhappiness, emptiness, and despair that come from facing situations that seem out of one's control -- the nightmare roommate, being laid off from a job, losing a loved one. It's also true that in most cases, this sadness can be overcome by a new perspective, trying better strategies, or simply allowing the passage of time to do its healing work. Depression can be impacted by one's beliefs, but there is a kind of depression that exists independently of one's perspective on life.
SUICIDAL TENDENCIES

Apart from this series of articles (which took me a good two years to publish), I've stopped sharing my depression with other people. It's annoying, because most people don't know how to listen and empathize. They want to jump in with a solution that, if implemented by nightfall, just might make a difference by daybreak. It's just more hassle than it's worth. Over time, I've gone from being someone with an intense need to belong, to not caring what people think about me at all. I'll often go out of my way to avoid anything deeper than transactional relationships. Once a social butterfly, you'll find me quite the hermit these days. As a consequence, while I was once open to sharing my feelings of loneliness and despair, I rarely mention them any more on social media and practically never to my IRL friends. I would be the last person to call a suicide hotline, by the way. Judge me if you wish, but I'm just being honest. If you want to know what is going on in the head of a severely depressed person with suicidal ideation, here's a least one brain you can peer into.
There's a general consensus that suicide is a selfish decision, even a cowardly act. This was a casual opinion of my own for years, as well. Not until suicide touches someone in your life -- or when you enter its despondent realm yourself -- does the ridiculousness of that notion becomes apparent. Understand that for a person to commit suicide, they have to overcome the brain's own strong predilection for self-preservation. It's not so easy to take the step of ending your life. Something has gone terribly wrong with the brain's ability to convincingly cry, "STOP!" for that to happen.
In my worst bout of depression, following the demise of long-term relationship, I reached the point where every waking moment was sheer misery. Some call this anhedonia -- the inability to feel pleasure. Normally, when we are feeling blue, we seek out something to stimulate our pleasure receptors. That's why ice cream, chocolate, and Reese's Peanut Butter Cups are popular go-tos for the bummed out. For me, it's always been music and movies. On this particular week, though, I had somehow lost the capacity to find any joy whatsoever in the usual pastimes. Anything that attempted to pacify my mood met with my contempt. The only thing I could do to escape the agony of just being alive and conscious was to sleep...and sleep I did. At first 8 hours a night, up from my usual 7. Then it advanced to 9, 10, 11, 12 hours. When dawn came, a wave of misery washed over my mind again.
Once, I woke up feeling so despondent that I knew with absolute clarity that I could end my life. Today, I could actually do it. Immediately upon this realization, I wept bitterly. I've not cried like that before or since. If anything, I've become more stoic about the idea of suicide. Don't get me wrong, my internal sense of self-preservation is still quite strong. The problem is that in moments of severe depression, that instinct is dampened. You'll do just about anything just to get rid of the feeling of misery making it unbearable to be awake.
DOOM AWAKENING

One of the most important developments in treating my depression, besides medication and therapy, was the discovery of doom. There's an old expression that misery loves company. I don't know about you, but when I listen to music it's not generally to cheer me up. No, I want my tunes to have a certain level of commiseration with what I'm feeling and going through at the time. When I discovered (quite by accident) Saint Vitus, I knew I'd found my soul food. I can't fully explain that eureka moment when Dave Chandler belted out that first downtuned note on the guitars on "Born Too Late" or when Wino joined with plaintive lyrics for "I Bleed Black." This resonated with me powerfully. It brought chills. This was medicine for my weary head, a kind of mental morphine to dull the pain. I'd come to the Roseland Theater for Down and left with Saint Vitus.
As a funny aside, my roommate (who accompanied me to the show) and I rehashed the bands of the night, giving our two cents on this or that. One thing he said still makes me smile a little inside. "What did you think of Saint Vitus?" I asked. "I don't think they're the kind of band that will withstand the test of time," he remarked. "Well," I rejoined, "they have been playing now for over 30 years and were the co-headliners on a national tour, so their sound must be resonating with a good number of people." Sure, it wasn't for everyone, but on that night my doom had come.
Every song on 'Born Too Late' (1986) so perfectly captures the malaise of the deeply wounded soul, not just in lyrics but in the whole vibe. There's a thick, smoky haze permeating the record and it reminds me a lot of what it feels like after you've poured out your heart until you've got no more tears left to cry. Come on, don't pretend you're so macho that normal human emotions elude you. It's hard to put doom into words, but I'll try: on the one hand you feel emotionally exhausted because you've emptied out all those pent up feelings of loss, fear, regret, and frustration, on the other hand there's a feeling of "reset" and it often makes things much clearer to sort through. For me, when I've exhausted all my emotional resources, I'm left with a feeling of blithe acceptance. A sense of being dealt a set of cards by the impartial hand of fate. That's the kind of vibe that Saint Vitus captures perfectly for me on this record.
youtube
I spent entire weekends on those long, wonderful rabbit trails of discovery. "Dying Inside" led me to Trouble's "The Tempter" with its oh-so-tragic central riff. Lyrically, the songs I was running across could not have been more apropos.
Pentagram, The Skull, and Candlemass were not lingering far behind. Then came the more recent monoliths of doom: Electric Wizard, Windhand, High on Fire, Burning Witch, Khanate, Pilgrim, Serpentine Path, Usnea, Demon Lung, Ancient VVisdom, Dopelord, and the NOLA sludge scene, along with lesser known but equally as powerful acts like Undersmile, Shepherd's Crook, Reptile Master, Purple Hill Witch, Witchthroat Serpent, March Funèbre, Beldam, Hooded Priest, Regress, and 71TONMAN (listen to the Spotify playlist).
Doom metal spoke to me with a sharp realism that I connected with immediately. When you have no strength left to get angry at the world, you switch your listening habits from Car Bomb to Cough. You can say, I suppose, that doom was my salvation. It kept me hanging on a little while longer. The salve of those slow, low riffs gave me a strange feeling of consolation. "We know life sucks, too. Welcome to reality." It's like being awakened to the Matrix, but feeling there's not a damned thing you can do to change any of it. Your fate is sealed. It's an honesty that is both refreshing and freeing, I suppose, though one does wish to reclaim the notion of hope.
Believe it or not, even after writing all of this, optimism is my default mode. When I'm feeling well, and even when my depression is at low levels, the needle always leans towards inspiration, creativity, even a mischievous sense of humor and an aw, shucks smile that people tend to notice. I don't want to be depressed. The problem is that severe depression can make you feel, illusion or not, like you're paralyzed from doing anything about it.
As I've experienced more and more cuts and scrapes of life, I've become increasingly numb to it all, like the massive build-up of scar tissue. Things that upset me easily in the past might still hurt, but I've come to expect them, so they have the impact of a dull table knife. Perhaps I'm becoming a nihilist, despite my optimistic tendencies. It's hard not to be. Don't worry about me, though. If anything, I want to stick around to see what's going to happen next. It's the inborn curiosity we all have inside of us -- the same thing that I imagine kept Stephen Hawking going for decades after being wrecked by a disease that cruelly mangled his body into its famously misshapen form, stealing away his most basic expressive freedoms -- save for the power of his eyes and the thoughts behind them.
I've also made a deliberate attempt to pursue treatment (both psychiatric and psychological care) for my depression, which I urge you to do if you are likewise laboring under its crushing weight. The perspective of time, coupled with a remedy for mind and body can have a significant impact on your perspective, if not your life circumstances.
THE WINDY ROAD AHEAD

Learn from your mistakes, don't dwell on them. Repeated affirmations like this one may seem trite, but they are ultimately true. You can be free from the chains of guilt and move forward, as one performer puts it, "from strength to strength."
Don't kill yourself (literally or metaphorically) for someone else or for someone else's decisions. It may bum you out that a roomie decided to take your money and run or that you were rebuffed by a long-time crush or made jobless through corporate-wide cuts. You don't own that, they do.
Walks
Get off the couch, move that bod. Something as simple as a walk down the block or a drive out of town can do wonders for your perspective. As a homeschool teen living under the strict rule of a radical fundamentalist household in rural East Texas, my one salvation were those long walks in the open field -- especially when my parents started having loud, intense fights related to my mom's own mental health. I sorted through so many of life's problems (most of which seemed much larger then than they do now) through those solitary, hour-long strolls.
I really miss that where I live now, in a more congested neighborhood, so I have to find other ways of getting away from it all (getting up and out a half-hour before the other walkers, for instance, helps). Even if I don't want to rustle myself awake and move around to do as simple a task as taking out the trash, sometimes the feeling...let me revise that...quite often the feeling follows after the decision has been made and the body is in motion.
Projects
Another piece of advice I have for coping with depression is to channel your frustrations in projects. When I'm depressed, I throw myself into my work. Hell, Doomed & Stoned started because I needed a project to pour myself into. My counselor asked me once, "If you woke up tomorrow without depression, what would be different about your world?"
She encouraged me to start with the things that were in my immediate vicinity. "Well, there wouldn't be mail strewn all over the floor. My dirty clothes would be in the hamper, my clean clothes folded and put away. I'd take the time to cook myself a meal, instead of running out the door eating a quick bite out of some package."
Good, let's make a list and start there. Do at least one of the things on your list between now and the time we meet again next week.
Talks
Despite my isolationist ways, I begrudgingly admit that talking often helps, too. Though I'm an introvert and am horrified at the idea of sharing my feelings with others, I've reached points in my depression where I was compelled to tell others about it. It's as natural to do that as to cry out when your body is experiencing jolting pain. I'm one of those verbal processors that tends to sort through my problems by talking to someone else. Often, pride or shame or lack of trust gets in the way of sharing with our family and friends, so at the very least the much talked about Suicide Prevention Hotline could actually help you gain perspective on your situation.
Journals
If you don't talk, at least journal. Again, I'm not a journaler and this is the first time in almost three decades that I've written about anything related to my depression. Role play with me. You're a scientist studying the human psyche. How would you describe those feelings you call depression? When I was first asked to describe it to a counselor, I found myself at a loss for words. She helped me with prompts:
Can you tell me what it feels like?
"I walk around feeling like a dark, thick raincloud is hovering all around me all the time."
Do you feel it in a part of your body?
"Well, yeah, I guess. The head. And the chest. It feels like there's pressure building from all around me, like my head is going to explode. My heart feels like it's going to leap out of my chest."
What's happening around you when these feelings arise?
I'd then go on to detail some recent happenings. She'd press me further to describe the kinds of thoughts racing through my head in these situations. All of this was really helpful in getting me to define this nebulous, gray malaise that was following me everywhere I went.
I don't keep a journal, per se. Something about it feels needlessly egotistical, a vain attempt to reinforce the illusion in our YouTube fame crazy world that my life is worth discovering and remembering at some point in the distant future. And yet, writing down one's thoughts can be another effective way of untangling that anxious ball of feelings that keeps me from thinking rationally about the depression I'm feeling.
Today is my birthday, but I couldn't care less. It's not about getting old. I stopped caring about that 10 years ago. It's something about celebration, specifically when the attention is on me. I can't adequately describe how contemptuous I find it. My last birthday was spent alone in an empty house and a bottle of Scotch, catching up with past seasons of Game of Thrones. I was so glad it was over and the happy birthday wishes stopped. There's nothing special about this day for me.
At some point, my family stopped celebrating birthdays and holidays. I'm not sure when it happened or why. Certainly not for religious reasons, more probably for financial ones. I grew up in a family that barely scraped by, so birthdays seemed a luxury we couldn't afford. Now, it just feels indulgent. More than that, it feels sad. It reminds me of all the disappointments, hurts, and failures of the past year. It's not as though it's all bad, of course. If nothing else my birthday gives the illusion that a chapter has turned, with new possibilities for the future. I also have to come to terms with how many people out there actually seem to care about me, maybe even love me.
And later that day, I forced myself to go to a show I was quite enthused about, but didn't factor in depression being the party pooper.
I can't account for what it is that comes over me. There are people here that genuinely like me, who probably even want to get to know me better, but I push them away. Not so much directly, but indirectly, by excusing myself to use the restroom and then changing my mind midway and just leaving the venue -- without even the courtesy of a "goodbye" to friends or a "great show" to the bands. I feel awful about it afterwards, but in that moment it's like a flood of emotional pain washes over me and it feels like I'm carrying an anchor chained around my neck. I feel the great urge to find my way to unlit corners. To look busy and preoccupied. Would it hurt me to say hello? To smile? Perhaps not, but right now my psyche is tingling like some kind of Spidey Sense telling me, "Get out of here! Just get your shit and leave...NOW."
As dour and hopeless as that may feel, just the act of writing it down afforded me a release, which incidentally I did not feel until the writing was all said and done.
Hope, a new beginning Time, time to start living Just like just before we died
youtube
Hurt, falling through fingers Trust, trust in the feeling There's something left inside There's no going back to the place we started from.
ONE MORE THING
For those of you who are wondering what you can do for a friend, family member, coworker or just someone you know casually from shows you both frequent, I couldn't say it better than one of my longtime fellow travelers in doom, who offered up this advice:
"While it's all very well and fucking dandy that there are so many people telling those who are struggling to reach out to them, I don't think people are quite understanding just how mental illness works sometimes. People quite often don't reach out, because those that are suffering from mental illness, at times, feel like they are a burden by unloading their shit onto someone else, despite the invitation to do so. It's generally the same concept that leads on to suicide.
I obviously can't speak for everyone, but I can speak for myself when I say the last thing I want to do is reach out to anyone because I feel like I am a burden and everyone would be better off without me -- and that is ultimately why I don't reach out. The point that I'm trying to get at is if you see someone struggling YOU reach the fuck out. If you don't see someone who used to be around, YOU reach the fuck out. Think about it. It's not that hard."
Well said and completely on the mark. At the same time, if you're feeling alone and uncared for, you may look at people’s lack of inquiry as more confirmation that you are worthless trash. You may interpret a busy person's slight as utter rejection. Don't worry about what others may or may not think of you. You need to take care of you, for you. The future is fickle. Your fortunes can change on a dime, so why base your self-worth and your decision about whether to live or die by how you feel right now? Ride it out, seek out help, get a game plan in play.
I say this as someone who knows how hard it can be to get mental health. I was double insured -- through my employer and the Veterans Administration -- and I couldn't get a god damned psychiatric appointment to reevaluate and adjust my meds. I called all over town trying to get in with someone. "Sorry, we're not accepting new patients" was the universal refrain. The VA would just be too many month's wait, I told myself, based upon how long it has taken me in the past to get a conventional medical appointment. In desperation, I called up my primary care doctor who asked if I was suicidal. For the first time in my life, I knew with full certainty the answer was yes. The more miserable I felt, the more I contemplated dying. If I did it, it would be something quick and sudden, I would daydream in my most despondent moment. "You need to check yourself into the hospital now," she told me adamantly. I did exactly that. I walked into the ER and told them I was suicidal. They led me to a room, had me take off all my clothes, and put on a hospital gown. I stayed in a padded room waiting for a social worker to see me. It was a desperate move, but it did pay off in getting me fast-tracked to see a psychiatrist.
One thing I learned about medication from my new psychiatrist (because he was very caring, very careful, and hence very effective at his job) is that everyone’s brain chemistry is uniquely different. There can be other issues impacting mood, too, such as thyroid, environmental stressors, sleep problems, vitamin deficiencies, and so on. Again, it’s often hard to see whether the cart is leading the horse or the horse is leading the cart, in terms of the mind-body connection. Long story short, this doctor adjusted my meds to near perfection to get me through the rare summer-long depression I was experiencing.
Just a few months later, he got hired away to work for the County and I was left back in the same boat once again. I got a great referral, but didn't realize until bills came in I couldn't pay that the doctor was out of my insurance network. Believe me, many people prefer to go without care entirely than to go into debt and I was one of them (truthfully, I still am). I went another year until I couldn't take it anymore and this time in my desperation reached back out to the VA. Surprisingly, they saw me within a week and prioritized my suicidal depression. I'm now in a good spot as a result, but it was a long, windy, uncertain road getting here. I know it's hard to find help. Sometimes you don't know what's available to you until you knock a little louder and get people's attention.
The older I get, it seems the more stubborn I am, particularly when it comes to reaching out and asking for help. Perhaps I've always been that way and am only now realizing it's become a liability. After taking off three weeks during the holidays to catch up with the many projects that were piling up around me, I realized that my depression was sometimes stronger than my will to power through and do my best work. I would find myself sitting at the computer for hours trying to get started with a story, trying to edit audio for a podcast, trying to prepare a team member's submission for publication, and every time I would find myself coming up against something painful, perhaps similar to the long recognized creative crimp known as writer's block. I describe it as an inhibitor chip in my brain that sends pain signals to my psyche whenever I contemplate moving forward.

Of course, rationally, I know it's all just a matter of the will, right? That's what those who aren't experiencing depression will tell you, at least. They don't want to go to the gym, but they make the choice to do it anyway, so why can't you just "man up" and do what needs to be done? Well, those aren't so much the messages other people give me, as they are my own conscience. The guilt itself from a day coming and going without results adds its own layer of complication to my mood. Thankfully, I have a wonderful counselor who understands and is helping me to tackle this with cognitive strategies. This, coupled with sensible medical treatment, has at least helped me to find "even flow" again.
Finally, you're going to have some bad days where you may even want to be productive, but your body feels like it's in revolt. As a creative person who loves to pour myself into as many projects as I can when I'm feeling good, it can be extraordinarily frustrating to not even feel the will to check email, open a letter, or listen to a stitch of music. Most days, I'm trying to work in concert with my body's natural rhythms. I'm more of a morning person and get my best work done between 8AM and 11AM. Anything after that is going to be hit or miss with diminishing returns. With that in mind, I have to hold back from starting new projects before the ones already on my plate are finished, because when I'm feeling good, I think I can take on the world.
This is all a part of me rediscovering what it's like to feel balanced, bright, and in love with life. It can be frustrating to have that feeling back, only to watch it wither away as the week progresses. Since I have very high expectations of myself, it's natural for me to heap guilt upon guilt for all the missed opportunities, but beating myself up only compounds the problem (it took me a long time to really get this about myself, too). Every day is a struggle, but I've decided I'm staying in the fight for the long haul.
In short: Be patient with yourself. Be fair with yourself. Be good to yourself. Remember, this too shall pass.
"Someday you're going to die, just like some day I'm going to die. But until then, you fight like hell to stay alive, you get that?!"
-- William Holden, The Earthling (1980)
#Closer To The End#Depression#Suicide#Doom#Metal#Saint Vitus#Trouble#Alice in Chains#Windhand#Doomed & Stoned
6 notes
·
View notes
Text
*Frequently Asked Questions About Seeing a Mental Health Professional*
There is a growing acceptance that mental health problems are common and there is a need to see mental health professionals, and receive expert care and interventions.
However, several misconceptions and questions continue to swirl around who needs to see a mental health professional? what should the expectations be? Who is a mental health professional? Is it overrated? Can’t I just wing it by myself? And so on.
In today´s article, we attempt to respond to some of these questions.
*Question:* Who needs to see a mental health professional?
*Answer:* Anyone and everyone may need to see a mental health professional if they are having difficulties with their thinking, mood (emotions), behaviour, sleep, interpersonal relationships, functioning, drug abuse, and so on; which is causing them distress or causing distress to others around them.
There may also be associated difficulties with their day to day functioning at work, with their families as well as their social life.
*Question:* Mental health professionals only see people who have mental illness or are mad
*Answer:* No this is not correct. Some people come into therapy to resolve problems with anxiety, family and interpersonal functioning, marital difficulties, self esteem issues, addictive behaviours, anger management issues and so on. Of course, some people also have diagnosable mental health challenges that may require specific treatments and interventions.
*Question:* What is the difference between a Coach, Psychologist and Psychiatrist? Are they all doing the same thing?
*Answer:* No, they are not doing the same thing, though some overlap certainly exists in that they all contribute towards helping individuals live a happier and more productive life.
*A Coach* is not a medically qualified professional, but is someone with training and certification to understand individual as well as organizational difficulties, and has the skills to guide and help them to overcome them. They serve as expert guides to help people actualize their life goals, meet their targets and be more productive.
However, for a coach to be effective, it pre-supposes that the client is in good health and there are no background mental health problems. They are increasingly very important to help individuals and organizations to become more productive and happier with themselves.
*A psychologist* is a professional who has had a first degree in the social sciences, usually in psychology, counselling or education; and has received postgraduate training at Masters and PhD level in the specialized field of clinical psychology.
Thus, they are experts at understanding human behaviour across the lifespan, understanding and detecting abnormalities in behaviour, personality or relationships. The specialization may also be in other fields of psychology, such as organizational psychology, sports psychology, developmental psychology etc.
But those commonly referred to as Therapists are those that have specialized in Clinical Psychology. They are especially adept at the use of psychological assessments and instruments for evaluating personality, intelligence quotients as well as provision of specialized therapies. They do not prescribe medications, because they are not medical doctors.
Therefore, when patients are severely ill, or those who are not getting better with therapy alone, they refer them to psychiatrists for additional use of medications.
*Psychiatrists* are medical doctors who have undergone postgraduate specialization in the field of psychiatry. Thus, they are medical specialists whose training also incorporates basic as well as clinical psychology; in addition to studying mental disorders and how to mange and treat them.
Thus, a psychiatrist is able to diagnose medical problems, identify mental health problems as well as provide treatment interventions that may include use of clinical psychology skills, as well as the prescription of medications where it is deemed necessary. Psychiatrists are relevant across the spectrum of mental health promotion, prevention, early identification and treatment of disorders as well as rehabilitation.
*Question:* Are coaches, psychologists and psychiatrists all mental health professionals?
*Answer:* No, coaches help with life issues and improving personal productivity towards the attainment of goals. Thus, they are often called Life Coaches. But they are not mental health professionals. Psychologists and Psychiatrists are mental health professionals.
*Question:* If I see a mental health professional for therapy, will they make all my problems to go away?
*Answer:* Mental health professionals do not wield a magic wand. You need to be actively engaged as they try to help you understand issues such as previous trauma, unresolved conflicts and negative patterns of thinking and responding to situations that may be causing distress and unhappiness in the here and now.
The overall goal is to gain insight into the unhelpful patterns of dealing with situations and learn better and more positive ways of thinking and responding to such situations.
And where there are identifiable mental health problems, to receive specific therapies and treatments (including use of medications where necessary) to facilitate recovery and gain mastery over addictions too.
*Jibril Abdulmalik*
Tribune Article for the column _“Your Mental Health & You”_
Thursday, 17th September 2020
*Asido Foundation*
www.asidofoundation.com
0 notes
Link
New AI Mental Health Tools Beat Human Doctors at Assessing Patients
11,627
About 20 percent of youth in the United States live with a mental health condition, according to the National Institute of Mental Health.
That’s the bad news.
The good news is that mental health professionals have smarter tools than ever before, with artificial intelligence-related technology coming to the forefront to help diagnose patients, often with much greater accuracy than humans.
A new study published in the journal Suicide and Life-Threatening Behavior, for example, showed that machine learning is up to 93 percent accurate in identifying a suicidal person. The research, led by John Pestian, a professor at Cincinnati Children's Hospital Medical Center, involved 379 teenage patients from three area hospitals.
Each patient completed standardized behavioral rating scales and participated in a semi-structured interview, answering five open-ended questions such as "Are you angry?" to stimulate conversation, according to a press release from the university.
The researchers analyzed both verbal and non-verbal language from the data, then sent the information through a machine-learning algorithm that was able to determine with remarkable accuracy whether the person was suicidal, mentally ill but not suicidal, or neither.
“These computational approaches provide novel opportunities to apply technological innovations in suicide care and prevention, and it surely is needed,” Pentian says in the press release.
In 2014, suicide was ranked as the tenth leading cause of death in the United States, but the No. 2 cause of death for people age 15 to 24, according to the American Association of Suicidology.
A study just published in the journal Psychological Bulletin further punctuated the need for better tools to help with suicide prevention. A meta-analysis of 365 studies conducted over the last 50 years found that the ability of mental health experts to predict if someone will attempt suicide is “no better than chance.”
“One of the major reasons for this is that researchers have almost always tried to use a single factor (e.g., a depression diagnosis) to predict these things,” says lead author Joseph Franklin of Harvard University in an email exchange with Singularity Hub.
Franklin says that the complex nature behind such thoughts and behaviors requires consideration of tens if not hundreds of factors to make accurate predictions. He and others argue in a correspondence piece published earlier this year in Psychological Medicine that machine learning and related techniques are an ideal option. A search engine using only one factor would be ineffective at returning results; the same is true of today’s attempts to predict suicidal behavior.
He notes that researchers in Boston, including colleague Matthew K. Nock at Harvard, have already used machine learning to predict suicidal behaviors with 70 to 85 percent accuracy. Calling the work “amazing,” Franklin notes that the research is still in the preliminary stages, with small sample sizes.
“The work by the Pestian group is also interesting, with their use of vocal patterns/natural language processing being unique from most other work in this area so far,” Franklin says, adding that there are also limits as to what can be drawn from their findings at this point. “Nevertheless, this is a very interesting line of work that also represents a sharp and promising departure from what the field has been doing for the past 50 years.”
Machine learning has yet to be used in therapy, according to Franklin, while most conventional treatments for suicide fall short.
“So even though several groups are on the verge of being able to accurately predict suicidality on the scale of entire healthcare systems [with AI], it’s unclear what we should do with these at-risk people to reduce their risk,” Franklin says.
To that end, Franklin and colleagues have developed a free app called Tec-Tec that appears effective at “reducing self-cutting, suicide plans, and suicidal behaviors.”
The app is based on a psychological technique called evaluative conditioning. By continually pairing certain words and images, it changes associations with certain objects and concepts, according to the website, so that within a game-like design, Tec-Tec seeks to change associations with certain factors that may increase risk for self-injurious behaviors.
“We’re working on [additional] trials and soon hope to use machine learning to tailor the app to each individual over time,” Franklin says, “and to connect the people most in need with the app.”
Catching schizophrenic speech
Last year, researchers in a study published in the journal Schizophrenia also had promising results in using machine-learning algorithms to predict later psychosis onset in high-risk youths.
Thirty-four participants were interviewed and assessed quarterly for two and a half years. Using automated analysis, transcripts of the interviews were evaluated for coherence and two syntactic markers of speech complexity—the length of a sentence and the number of clauses it contained.
The speech features analyzed by the computer predicted later psychosis development with 100 percent accuracy, outperforming classification from clinical interviews, according to the researchers.
“Recent developments in computer science, including natural language processing, could provide the foundation for future development of objective clinical tests for psychiatry,” they wrote.
Diagnosing ADHD early
In a project now under way, scientists at the University of Texas at Arlington and Yale University will combine computing power and psychiatric expertise to design an AI system that can assess a common disorder among youth: attention-deficit/hyperactivity disorder (ADHD), which the Centers for Disease Control and Prevention (CDC) says affects 8.5 percent of children ages 8 to 15.
The research uses “the latest methods in computer vision, machine learning and data mining” to assess children while they are performing certain physical and computer exercises, according to a press release from UTA. The exercises test a child’s attention, decision-making and ability to manage emotions. The data are then analyzed to determine the best type of intervention.
"We believe that the proposed computational methods will help provide quantifiable early diagnosis and allow us to monitor progress over time. In particular, it will help children overcome learning difficulties and lead them to healthy and productive lives,” says Fillia Makedon, a professor in UTA’s Department of Computer Science and Engineering.
Keeping an eye out for autism
Meanwhile, a group at the University of Buffalo has developed a mobile app that can detect autism spectrum disorder (ASD) in children as young as two years old with nearly 94 percent accuracy. The results were recently presented at the IEEE Wireless Health conference at the National Institutes of Health.
The app tracks eye movements of a child looking at pictures of social scenes, such as those showing multiple people, according to a press release from the university. The eye movements of someone with ASD are often different from those of a person without autism.
About one in 68 children in the United States has been diagnosed with ASD, according to the CDC. The UB study included 32 children ranging in age from two to 10. A larger study is planned for the future.
It takes less than a minute to administer the test, which can be done by a parent at home to determine if a child requires professional evaluation.
“This technology fills the gap between someone suffering from autism to diagnosis and treatment,” says Wenyao Xu, an assistant professor in UB’s School of Engineering and Applied Sciences.
Technology that helps treat our most vulnerable populations? Turns out, there is an app for that.
Image Credit: Shutterstock
4 notes
·
View notes
Text
What It's Like to Learn You're Going to Die
Nessa Coyle calls it “the existential slap”—that moment when a dying person first comprehends, on a gut level, that death is close. For many, the realization comes suddenly: “The usual habit of allowing thoughts of death to remain in the background is now impossible,” Coyle, a nurse and palliative-care pioneer, has written. “Death can no longer be denied.”
I don’t know exactly when my mother, who eventually died of metastatic breast cancer, encountered her existential crisis. But I have a guess: My parents waited a day after her initial diagnosis before calling my brother, my sister, and me. They reached me first. My father is not a terribly calm man, but he said, very calmly, something to this effect: “Your mother has been diagnosed with breast cancer.”
There was a pause, and then a noise I can best describe as not quite a sob or a yell, but feral. It was so uncharacteristic that I didn’t know then, and I still don’t know, whether the sound came from my father or my mother.
I think that was the moment of her—and their—existential slap.
For many patients with terminal diseases, Coyle has observed, this awareness precipitates a personal crisis. Researchers have given it other names: the crisis of knowledge of death; an existential turning point, or existential plight; ego chill. It usually happens as it did with my mother, close to when doctors break the news. Doctors focus on events in the body: You have an incurable disease; your heart has weakened; your lungs are giving out. But the immediate effect is psychological. Gary Rodin, a palliative-care specialist who was trained in both internal medicine and psychiatry, calls this the “first trauma”: the emotional and social effects of the disease.
The roots of this trauma may be, in part, cultural. Most people recognize at an intellectual level that death is inevitable, says Virginia Lee, a psychologist who works with cancer patients. But “at least in Western culture, we think we’re going to live forever.” Lee’s advanced-cancer patients often tell her they had thought of death as something that happened to other people—until they received their diagnosis. “I’ve heard from cancer patients that your life changes instantly, the moment the doctor or the oncologist says it’s confirmed that it is cancer,” she says.
The shock of confronting your own mortality need not happen at that instant, Coyle notes. Maybe you look at yourself in the mirror and suddenly realize how skinny you are, or notice your clothes no longer fit well. “It’s not necessarily verbal; it’s not necessarily what other people are telling you,” Coyle says. “Your soul may be telling you, or other people’s eyes may be telling you.”
E. Mansell Pattison, one of the early psychiatrists to write about the emotions and reactions of dying people, explains in The Experience of Dying why this realization marks a radical change in how people think about themselves: “All of us live with the potential for death at any moment. All of us project ahead a trajectory of our life. That is, we anticipate a certain life span within which we arrange our activities and plan our lives. And then abruptly we may be confronted with a crisis ... Whether by illness or accident, our potential trajectory is suddenly changed.”
In this crisis, some people feel depression or despair or anger, or all three. They grieve. They grapple with a loss of meaning. A person’s whole belief system may be called into question because “virtually every aspect of their life will be threatened by changes imposed by the [disease] and its management,” Lee has written. In a small 2011 Danish study, patients with an incurable esophageal cancer reported that after their diagnosis, their lives seemed to spin out of control. Some wondered why they had received a fatal diagnosis, and fell into despair and hopelessness. “I didn’t care about anything,” one patient said. “I had just about given up.”
In the 1970s, two Harvard researchers, Avery Weisman and J. William Worden, did a foundational study on this existential plight. Newly diagnosed cancer patients who had a prognosis of at least three months were interviewed at several different points. At first, for almost all the patients in the study, existential concerns were more important than dealing with the physical impacts of disease. The researchers found that the reckoning was jarring, but still relatively brief and uncomplicated, lasting about two to three months. For a few patients, the crisis triggered or created lasting psychological problems. A few others seemed to face the crisis, then return to a state of denial, and then double back to the crisis—perhaps more than once. In the study, the researchers describe a patient who was told her diagnosis, only to report to interviewers that she didn’t know what it was—and then make it clear she wasn’t interested in receiving a diagnosis in the near future.
Palliative-care doctors used to think that a patient was either in a state of denial or a state of acceptance, period, Rodin says. But now he and his colleagues believe people are more likely to move back and forth. “You have to live with awareness of dying, and at the same time balance it against staying engaged in life,” he says. “It’s being able to hold that duality—which we call double awareness—that we think is a fundamental task.”
Whether or not people are able to find that balance, the existential crisis doesn’t last; patients can’t remain long in a state of acute anxiety. Coyle has found in her work that later peaks of distress are not usually as severe as that first wave. “Once you’ve faced [death] like that once, it’s not new knowledge in your consciousness anymore,” she says.
The existential slap doesn’t always entail mental suffering, and medical professionals who work with the dying say there are rare cases in which patients seem to skip this phase altogether, or at least experience it in a much less painful way. “People can gradually come to the realization,” Coyle says. “No one has to go through the sudden shock of awareness.”
But for most, figuring out how to adapt to living with a life-threatening disease is a difficult but necessary cognitive process, according to Lee. When patients do emerge on the other side of the existential crisis, she finds that many are better off because of it. These patients are more likely to have a deeper compassion for others and a greater appreciation for the life that remains.
To arrive there, they have to squarely face the fact that they’re going to die. “If you’re an avoidant person, and you don’t like to think about these things, that works better when life is going well,” Rodin says. “It just doesn’t work well in this situation because reality doesn’t allow it. It’s like trying to pretend you don’t need an umbrella or something, or it’s not raining, when it’s pouring. You can do that when it’s drizzling, but eventually, you have to live with the rain.”
from Health News And Updates https://www.theatlantic.com/health/archive/2017/11/the-existential-slap/544790/?utm_source=feed
0 notes
Text
What It's Like to Learn You're Going to Die
Nessa Coyle calls it “the existential slap”—that moment when a dying person first comprehends, on a gut level, that death is close. For many, the realization comes suddenly: “The usual habit of allowing thoughts of death to remain in the background is now impossible,” Coyle, a nurse and palliative-care pioneer, has written. “Death can no longer be denied.”
I don’t know exactly when my mother, who eventually died of metastatic breast cancer, encountered her existential crisis. But I have a guess: My parents waited a day after her initial diagnosis before calling my brother, my sister, and me. They reached me first. My father is not a terribly calm man, but he said, very calmly, something to this effect: “Your mother has been diagnosed with breast cancer.”
There was a pause, and then a noise I can best describe as not quite a sob or a yell, but feral. It was so uncharacteristic that I didn’t know then, and I still don’t know, whether the sound came from my father or my mother.
I think that was the moment of her—and their—existential slap.
For many patients with terminal diseases, Coyle has observed, this awareness precipitates a personal crisis. Researchers have given it other names: the crisis of knowledge of death; an existential turning point, or existential plight; ego chill. It usually happens as it did with my mother, close to when doctors break the news. Doctors focus on events in the body: You have an incurable disease; your heart has weakened; your lungs are giving out. But the immediate effect is psychological. Gary Rodin, a palliative-care specialist who was trained in both internal medicine and psychiatry, calls this the “first trauma”: the emotional and social effects of the disease.
The roots of this trauma may be, in part, cultural. Most people recognize at an intellectual level that death is inevitable, says Virginia Lee, a psychologist who works with cancer patients. But “at least in Western culture, we think we’re going to live forever.” Lee’s advanced-cancer patients often tell her they had thought of death as something that happened to other people—until they received their diagnosis. “I’ve heard from cancer patients that your life changes instantly, the moment the doctor or the oncologist says it’s confirmed that it is cancer,” she says.
The shock of confronting your own mortality need not happen at that instant, Coyle notes. Maybe you look at yourself in the mirror and suddenly realize how skinny you are, or notice your clothes no longer fit well. “It’s not necessarily verbal; it’s not necessarily what other people are telling you,” Coyle says. “Your soul may be telling you, or other people’s eyes may be telling you.”
E. Mansell Pattison, one of the early psychiatrists to write about the emotions and reactions of dying people, explains in The Experience of Dying why this realization marks a radical change in how people think about themselves: “All of us live with the potential for death at any moment. All of us project ahead a trajectory of our life. That is, we anticipate a certain life span within which we arrange our activities and plan our lives. And then abruptly we may be confronted with a crisis ... Whether by illness or accident, our potential trajectory is suddenly changed.”
In this crisis, some people feel depression or despair or anger, or all three. They grieve. They grapple with a loss of meaning. A person’s whole belief system may be called into question because “virtually every aspect of their life will be threatened by changes imposed by the [disease] and its management,” Lee has written. In a small 2011 Danish study, patients with an incurable esophageal cancer reported that after their diagnosis, their lives seemed to spin out of control. Some wondered why they had received a fatal diagnosis, and fell into despair and hopelessness. “I didn’t care about anything,” one patient said. “I had just about given up.”
In the 1970s, two Harvard researchers, Avery Weisman and J. William Worden, did a foundational study on this existential plight. Newly diagnosed cancer patients who had a prognosis of at least three months were interviewed at several different points. At first, for almost all the patients in the study, existential concerns were more important than dealing with the physical impacts of disease. The researchers found that the reckoning was jarring, but still relatively brief and uncomplicated, lasting about two to three months. For a few patients, the crisis triggered or created lasting psychological problems. A few others seemed to face the crisis, then return to a state of denial, and then double back to the crisis—perhaps more than once. In the study, the researchers describe a patient who was told her diagnosis, only to report to interviewers that she didn’t know what it was—and then make it clear she wasn’t interested in receiving a diagnosis in the near future.
Palliative-care doctors used to think that a patient was either in a state of denial or a state of acceptance, period, Rodin says. But now he and his colleagues believe people are more likely to move back and forth. “You have to live with awareness of dying, and at the same time balance it against staying engaged in life,” he says. “It’s being able to hold that duality—which we call double awareness—that we think is a fundamental task.”
Whether or not people are able to find that balance, the existential crisis doesn’t last; patients can’t remain long in a state of acute anxiety. Coyle has found in her work that later peaks of distress are not usually as severe as that first wave. “Once you’ve faced [death] like that once, it’s not new knowledge in your consciousness anymore,” she says.
The existential slap doesn’t always entail mental suffering, and medical professionals who work with the dying say there are rare cases in which patients seem to skip this phase altogether, or at least experience it in a much less painful way. “People can gradually come to the realization,” Coyle says. “No one has to go through the sudden shock of awareness.”
But for most, figuring out how to adapt to living with a life-threatening disease is a difficult but necessary cognitive process, according to Lee. When patients do emerge on the other side of the existential crisis, she finds that many are better off because of it. These patients are more likely to have a deeper compassion for others and a greater appreciation for the life that remains.
To arrive there, they have to squarely face the fact that they’re going to die. “If you’re an avoidant person, and you don’t like to think about these things, that works better when life is going well,” Rodin says. “It just doesn’t work well in this situation because reality doesn’t allow it. It’s like trying to pretend you don’t need an umbrella or something, or it’s not raining, when it’s pouring. You can do that when it’s drizzling, but eventually, you have to live with the rain.”
Article source here:The Atlantic
0 notes