#yes i know blood typing was discovered only 4 years after Dracula was published
Text
Bram Stoker: well i only befriend and propose to people with the same blood type as me so i don't see a problem
#yes i know blood typing was discovered only 4 years after Dracula was published#i just love the idea of everyone in the Dracula-hunting polycule all having the same blood type because Bram thinks that's Very Normal#let me have this#dracula daily#dracula#re: dracula#dracula memes#bram stoker
236 notes
·
View notes
Text
Some statistics on Lucy and the odds of surviving (non-vampiric) blood transfusions
Because it’s Dracula-season again, and because I am absolutely that kind of nerd, I spent some time calculating the actual odds of Lucy surviving all those blood transfusions from unrelated donors. To summarise what I found up front: Lucy's odds aren't great, but they're still a lot higher than you might think.

Now, I’m not the first person ever to tackle this question, and having no medical qualifications whatsoever, I'm not the best person either. But figuring out the answer to my own satisfaction was a great excuse to learn a whole lot of fascinating stuff that took some digging to figure out, so (with the caveat that I am entirely open to corrections from real professionals) naturally now I want to share it.
The complete world history of attempted blood transfusions is way beyond scope for us here (you can find plenty of sources on it online if you’re curious). But as Stoker’s text aptly demonstrates, the science of blood transfusion had come a long way by the Victorian era – just not the means for doctors to reliably predict which transfusions would be successful, and which would simply kill the patient. The principle behind the basic A, B and O blood types wouldn’t be discovered until 1900 – 4 years after Dracula was published, and wouldn't become part of general medical practice for much longer – and the additional Rh-factors wouldn’t be discovered until 1939. In Stoker's day, doctors were still so far behind the ball some of them thought transfusing milk into people suffering blood loss was a good idea (yes, really). And though I'm focusing on blood groups here, it goes without saying there are plenty of other risks that come from letting any Victorian-era doctor open your veins.
That said, what the average person knows about how blood types work may not be all that much advanced today from what doctors knew in the 1890s. It’s easy to come out of Dracula thinking, “Wow, they gave Lucy blood from four different people? The odds all their blood types would matched hers must be minuscule!” (and a quick search of the web for this topic will find people asking exactly that). But there are several factors which make Lucy’s chances a whole lot better than they might look on paper.

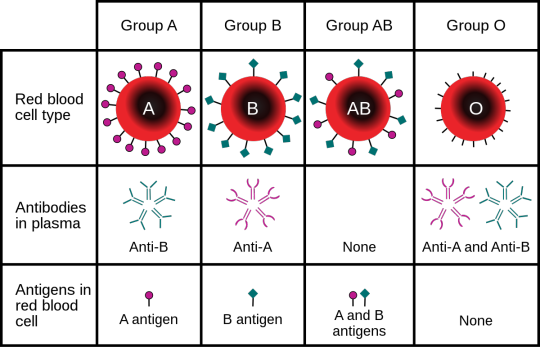
(Image source)
For one thing, even though there are many different blood groups to worry about, some are much more common than others. If just one blood group accounts for half the population (which is actually true of some countries), then Lucy’s odds of hitting four donors with the same group just by chance would go way up.
But far more important is the fact that blood groups don’t have to be a 'match' to be compatible. If Lucy is one of the 2% of the British population with the blood group AB+, she’d be a universal recipient – theoretically capable of receiving blood from anyone without adverse reactions. Similarly, if any of her donors were O-, she’s in luck again, because that makes them a universal donor. If Lucy herself is O-, however, she’s in trouble: universal donors can donate to any other group, but they can only receive from other O-negs.
Confused? Time to get a bit more technical.
When receiving blood, your greatest enemy is your own immune system. Vital as all those immune cells are, they are not smart, and have no way of knowing that all this foreign blood suddenly flooding your system is friendly. If the don’t recognise those blood cells, they’ll attack them, bonding to their surface and causing cells to clump together and form clots which can clog up your arteries and kill you. Transfusing the wrong blood type can and likely will kill you.
The immune system identifies blood cells as intruders via specific antigens found on the cell’s surface. The most important antigens in blood matching systems are the A and B antigens, and secondarily the Rhesus antigens (marked + or -). Some people have all of these antigens (AB+), some have none (O- with the ‘O’ more literally indicating a ‘0’ or a null) and many have some but not all (A+, B-, O+, etc). Meanwhile, the immune system of the recipient body, much like your racist uncle, will attack most anything with distinguishing features it hasn't seen before (like I said, it’s not smart). A blood cell which is missing a familiar antigen will slip through, but a blood cell sporting an unfamiliar antigen will trigger a reaction. So the immune system of someone with B-type blood will have issues with any A-type blood you try and transfuse in, but will be just fine with B or O, since O lacks any antigens to mark it as an intruder.
Once you know what you’re looking for, A, B, AB and O type blood can be identified fairly easily, just by mixing blood or antibodies and watching the reaction. I’ve seen some suggestions that this may have been understood even to some of the better-informed doctors in Victorian times: when unsure if a transfusion would be safe, they could try transfusing just a small amount of blood, watch for a bad reaction, and continue only if things look good. If you absolutely have to do a blood transfusion without any testing though, an immediate family member is your best bet: blood types can still differ among a family, but there’s a strong genetic component. (Sadly, this wouldn’t have been an option for Lucy, as her mother was already unwell, and would not have been considered a good transfusion candidate.)
Things get more complicated when you add in the Rhesus factor, which wasn’t discovered until some decades later, and for good reason: bad reactions to Rh+ blood develop in Rh- people only after that first transfusion. While A and B types might be like your racist uncle, the Rh factor is more like putting a dog on your basketball team: you’ll get away with it once, because you’ve brought in something so unexpected no-one’s made a rule about it yet (let alone bothered to come up with anti-dog basketball tactics). Unlike the standard A and B antigens, the immune system has to have 1) seen Rh+ blood, and 2) spent some time thinking about a good plan of attack before it’s ready to do anything about it – by which point the donor blood should be out of your system anyway. It's only the next transfusion after that where you can hit problems.
In practice, the Rh factor is of most concern to Rh- mothers carrying Rh+ babies. The first baby should be fine, but the delivery process can result in some mixing of the mother and baby's blood ‒ and that can leave her immune system primed to take offense at any future passengers of the Rh+ persuasion (why this apparently doesn’t also apply to A and B type babies in A or B negative mothers I’m not sure, but obviously the Rh-immune response works differently). With all today’s modern medical technology, this is something doctors can identify in expectant parents and manage with medication, but obviously they're still going to want to avoid transfusing Rh+ blood into an Rh- patient (especially if they’ve already got Rh+ kids).
Regardless, for our purposes, it’s only from the second transfusion that the Rh factor could trip you up. So could that be an issue for Lucy, if she’s getting so many transfusions? It's harder to find good info on exactly how long the Rh immune reaction takes to develop after the first transfusion, but most of what I could find suggests we’re looking at a period of weeks to months at least. So that’s good news for Lucy: we can ignore Rh factors when we’re calculating her odds of survival.
As a minor aside here, the standard eight blood types you can get by combining A, B and the Rhesus factor aren’t technically the only blood types out there. These three antigens matter most because people both with and without them are common in the broader human population, but a small minority of people are missing other antigens that the rest of us get as standard. European blood banks apparently also classify blood by a Kell factor, and people with anaemia and other conditions likely to require regular transfusions may be checked for several other potential Rh-like issues. A handful of people worldwide have blood classified as neither Rh+ or Rh-, but Rh-null – missing antigens common to 99.9% of the human population, and being in that class is a very mixed blessing. Blood donations from someone Rh-null can be used in recipients with rare blood types that would make them incompatible with almost any other donor. But if someone Rh-null ever needs a blood donation themselves, they’re in big trouble.
So, enough theory. What’s all this mean for Lucy’s odds of making it through 4 blood transfusions from unrelated donors?
Unsurprisingly, ratios of different blood groups vary a lot country to country and population to population, so I looked up ratios in modern Britain (Van Helsing is Dutch, of course, but blood groups in the Netherlands are similar enough to those in the UK that we’ll ignore that, just for simplicity). It’s possible these ratios have drifted since Victorian times, but figuring out how is so far beyond scope here we’re not going to worry about it. As discussed above, we’ll also ignore Rh factors – Lucy’s almost certainly never had a blood transfusion or a baby before, and everything happens far too fast for an Rh-immune response to kick in.
Alright. It’s statistics time!
We don't know Lucy's blood group, so any are possible. For each potential Lucy-blood-group, we can generate a list of blood groups which will be compatible donors (we'll call that list C(x)), and from that, we can calculate the probability that she'll be compatible with any randomly-selected donor. For Lucy to survive, we need her to survive 4 successive blood transfusions, so we’re raising that survival probability to the power of 4. Then to calculate her overall probability of survival, we multiply the survival rate by the odds she’s in that blood group, and add them together (no need to divide by the total population, that’s an easy 100%). So if we let n = number of transfusions and P(x) = probability a person is in blood group x, we get the following lovely equation:

(Yes, I know, I'm sorry ‒ someone out there is going to want to check my working, and I like to be transparent.)
And with that, (assuming I’m not just talking out of my arse with all those calculations), that suggests Lucy’s overall chances of surviving 4 different blood transfusions is about: (drum roll)... 27%. So, roughly 1 in 4.
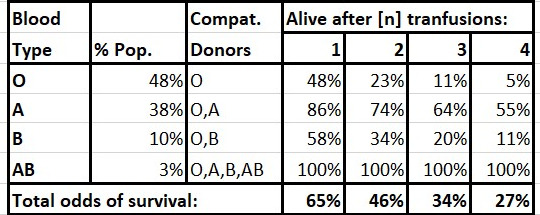
The really savvy reader might notice that Lucy does not, technically, survive all four transfusions – she dies shortly after the fourth, so it’s conceivable that last transfusion was a mismatch. If we take the requirements down to where Lucy only needs to survive 3 transfusions, her odds go up to 34%, or closer to 1 in 3. Still not great, but given the sorts of crazy one-in-a-million coincidences all fiction is built on, that’s actually pretty reasonable. Even if you do factor in Rh compatibilities, we're still looking at around 21% survival rate after 4 transfusions, which are pretty decent odds in the world of Victorian medicine.
Do those odds sound a little high to you? Here’s something to keep in mind. On paper, Lucy’s odds of surviving even a single random-donor transfusion are only 65%. But given she survived that first transfusion, the odds go up that she’s in one of those near-universal blood groups, and they keep going up. Sure, every new transfusion has a new chance to kill you, but statistically speaking, every transfusion you survive marks you as someone who’s a little more likely to survive the next. So someone who's already survived 2 transfusions has a 76% chance of surviving a 3rd ‒ and if they do survive that 3rd, an 80% chance of surviving a 4th.
As another aside though, even after surviving four successive transfusions, the odds Lucy’s in that lucky AB universal-recipient category are still only about 10% (compared to 3% of the base population). Statistically, it’s still far more likely she’s in the A-group ‒ the second largest group in the UK, and who can receive blood from the other largest group (O), letting them receive blood from a whooping 86% of the population without issue. Aren’t statistics wonderful?
Oh, all right – I’ll stop with the maths. We’ve made our point here.
Now, we could still point out that, for a supposedly-experienced physician, Stoker's Van Helsing seems pretty blase about the possibility his blood transfusions could backfire horribly ‒ but then, Lucy's already on death's door each time he resorts to asking for volunteers. He's doing the only thing that might save her life (and it does, until it doesn't).
To conclude, no-one is going to tell you Dracula makes sense. This is a book which offers no explanation for why Dracula should just happen land in England on the same town where his solicitor’s fiancée just is taking a holiday, let alone the rest of it. And Stoker had no way of knowing Lucy’s actual odds of surviving such a very Victorian procedure. But that whole blood transfusion sequence is far from being the least probable thing in the book.
111 notes
·
View notes