#PPROM
Photo
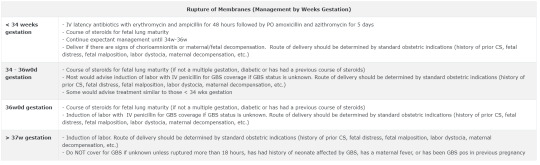
Like I have said before: I don’t like the term “premature rupture of membranes (PROM)” because when I hear “premature,” it just makes me think the baby is premature. But in PROM, “premature” means the membranes rupture prematurely, i.e., before labor starts. A better way to call it is “prelabor rupture of membranes.” If you use “prelabor” rather that “premature,” then you won’t confuse PROM with PPROM. PPROM = Preterm Premature Rupture of Membranes, which is more aptly “Preterm Prelabor Rupture of Membranes.” In the case of PPROM, baby is premature (i.e., not full term). They need to just make that standard.🙄
I'm not sure if the table is saying to give abxs in PPROM less than 34 weeks even if no signs of chorioamnionitis. So I sent a comment and will hopefully hear back soon.
3 notes
·
View notes
Text
When abortion was legal across the country, doctors in all states would typically offer to induce or perform a surgical procedure to end the pregnancy when faced with a pre-viability PPROM case — which is the standard of care, according to the American College of Obstetricians and Gynecologists (ACOG), and an option that many women choose. Especially before the 20-week mark, a fetus is extremely unlikely to survive without any amniotic fluid. But in the 18 states where abortion is banned before fetal viability, many hospitals have been turning away pre-viability PPROM patients as doctors and administrators fear the legal risk of terminating even a pregnancy that could jeopardize the mother’s well-being, according to 12 physicians practicing in antiabortion states.
—Caroline Kitchener on how new antiabortion laws are putting women's lives at risk
1 note
·
View note
Text
Premature rupture of membranes PROM
Everything you need to know about premature rupture of membranes
What is PROM- premature rupture of membranes
Premature rupture of membranes (PROM) is a term used to describe a situation in which a pregnant woman’s amniotic sac, also known as the “water bag”, breaks earlier than expected during labor. This can happen anywhere from weeks before labor up to just before labor begins, and is considered a potentially serious complication during pregnancy.
PROM can increase the risk of infection and other complications, and it can also lead to preterm labor. It is important for pregnant women to know the signs of PROM so that they can receive medical attention as quickly as possible if it occurs, as the earlier it is diagnosed the greater the chance for a successful outcome.
In this blog post, we will go over what PROM is, what the signs and symptoms are, and what the potential complications and risks are associated with it.
What is PPROM preterm premature rupture of membranes
Preterm Premature Rupture of Membranes (PPROM) is a clinical complication that occurs when membranes surrounding the fetus rupture prior to the beginning of labor.
This is a potentially serious consequence for both mother and baby, as it increases the risk of infection, preterm labor, and other complications. It is important for clinicians to detect the onset of PPROM early in order to ensure that the mother is given the necessary care and medication to reduce the risks associated with the condition.
Additionally, early detection can help ensure that the baby is delivered as quickly as possible while minimizing the chances of adverse outcomes. While there is no known definitive cause of PPROM, there are certain risk factors that increase the chances of it occurring, including cigarette smoking, intrauterine infection, and maternal age.
It is important for clinicians to be aware of these risk factors to ensure they can

What happens if I break my water before my labor starts
If you suspect your water has broken before labor has started, it is important to contact your healthcare provider right away. While it is possible to deliver a healthy baby if your water breaks before labor, there is a greater risk of infection for both you and your baby.
Your healthcare provider will likely want to monitor the situation and may advise you to come to the hospital for further observation and testing. Depending on your situation and the results of any tests, your healthcare provider may decide to induce labor or wait for labor to start naturally.
Regardless, it is important to follow your healthcare provider’s instructions. You may also wish to discuss any questions or concerns with your healthcare provider.
What happens if I break my water before term
If your water breaks before term, it is important to seek medical attention immediately. Depending on the circumstances, your healthcare provider may recommend that you be admitted to the hospital.
If the amniotic fluid is clear, you may be able to remain at home and wait for labor to start. If the amniotic fluid is not clear, your provider may recommend antibiotics to reduce the risk of infection for you and your baby.
Depending on the gestational age of your baby, your provider may also recommend that you receive steroids to help speed up your baby's lung development. Overall, preterm labor can be a very unpredictable and scary experience. Therefore, it is important to seek medical care if your water breaks before term.
Ultimately, PPROM is a rare but very difficult situation that can put both mother and baby at serious risk. If you experience PPROM before labor starts, you should contact your doctor immediately and discuss your treatment options.
Depending on your doctor's advice and the health of the baby, you may be induced or allowed to go into labor naturally. It's important to pay close attention to your symptoms and act quickly if you experience PPROM before your due date.
Read the full article
#birth#Hypno-Baby#naturalbirth#PPROM#prematureruptureofmembranes#pretermprematureruptureofmembranes#PROM
1 note
·
View note
Text
I don't know that I like third year. It's an adjustment. I'm sure it will be fine, eventually. But it's hard, and it's a different vibe, and it's struggling to find my place.
Looking at the interns, I do see how far I've come. I was in their shoes, once: struggling to find a cervix, falling behind with inductions/mag notes/strip notes/postpartum calls, scared of decelerations, unsure how to piece the clinical picture of labor together. I'm efficient with things I know how to do. Keep me to ante/gyne and I'm ON TOP of blood pressures, blood sugars, consults, antepartum calls etc. I feel pretty good about up-titrating blood pressure medications, deducing superimposed preeclampsia from chronic hypertension exacerbations, managing PPROM +/- PTL. I've read a lot. I think my signouts are decent.
But now as a third year, the antepartum "chief", I am really, really struggling. Now I have to delegate. I need to figure out what things I do, what things I have the second year do. When my actual R4 L&D chief is off the floor, I'm then in charge of everything (including training the day 3 intern). What's REALLY hard is the power dynamics. I'm in charge of the antepartum service, but my R4 is still in charge of me. And then on top of that, different R4s have different opinions, and then I get caught in the middle!!! A patient came into triage today, ruptured with twins, concern for preterm labor. I was told to let the R2 see her. I did, then sent the R2 home. Then the night team told me I should have seen her instead. And the R2 should be doing XYZ. And my signout wasn't well-prepared enough about her (even though I thought it was decent). Which to the first point, like, fair. I tried to have my R2 doing the XYZ. But I was also told to have her see the triage patient. So then it's like I'm in charge, but actually I'm in "charge", and the different people who are ACTUALLY in charge have different ideas about how to do things, but then it's either I take the blame or throw someone else under the bus.
And obviously, there are learning points. I can always know more about the patients. I think I did a fine job, especially since I've been on MFM/antepartum for TWO MONTHS STRAIGHT, but I do need to know the patients I don't admit a little better. And when my R4 can't come to signout, I really should know the floor better. These are things that will come with time, I'm sure. I am three days into my first time being a senior. I'm learning not only how to cover an ENTIRE service, but also how to manage an intern who needs to learn, well, literally everything. And can't do anything by herself yet. (Like I said, it's fine, we were all there at some point.)
But it's really, really hard to be told to do your job different ways from different people, and then you have to take responsibility for it anyway, and also you're supposed to be in charge of a service but you're not really.
And also, I have tomorrow off, but there's still hot as fuck drying equipment all over my apartment, and it's ninety degrees in here, and I can't play PC games without tripping the breaker. So I guess I'll just sit alone in the heat and be miserable.
Oh well. I ranted to like. Three of my friends. And here. I'll feel better eventually. Residency is really hard, and in really unexpected ways.
7 notes
·
View notes
Text
Two pregnant women with PPROM were denied care after Florida banned abortion - The Washington Post
https://www.washingtonpost.com/politics/2023/04/10/pprom-florida-abortion-ban/
When abortion was legal across the country, doctors in all states would typically offer to induce or perform a surgical procedure to end the pregnancy when faced with a pre-viability PPROM case — which is the standard of care, according to the American College of Obstetricians and Gynecologists (ACOG), and an option that many women choose. Especially before the 20-week mark, a fetus is extremely unlikely to survive without any amniotic fluid.
But in the 18 states where abortion is now banned before fetal viability, many hospitals have been turning away pre-viability PPROM patients as doctors and administrators fear the legal risk that could come with terminating even a pregnancy that could jeopardize the mother’s well-being, according to 12 physicians practicing in antiabortion states.
The medical exceptions to protect the life of the mother that are included in abortion bans are often described in vague language that does not appear to cover pre-viability PPROM, doctors said. That’s because the risks of the condition are often less clear-cut than other medical emergencies, such as an ectopic pregnancy, in which a fertilized egg grows outside of the uterus, dooming the fetus and posing an immediate danger to the mother’s life.
A 2022 study on the impact of Texas’s six-week abortion ban found that 57 percent of pre-viability PPROM patients in Texas who were not given the option to end their pregnancies experienced “a serious maternal morbidity,” such as infection or hemorrhage, compared with 33 percent of PPROM patients who chose to terminate in states without abortion bans. According to 2018 ACOG guidance, “isolated maternal deaths due to infection” have been reported in early PPROM cases.
Florida’s abortion law, enacted last year, bans the procedure after 15 weeks of pregnancy except when an abortion would either “save the pregnant woman’s life” or “avert a serious risk of substantial and irreversible physical impairment of a major bodily function.” The law includes another exception for a “fatal fetal anomaly,” which generally would not apply in a pre-viability PPROM case, according to several doctors, because there is no fetal anomaly but a lack of amniotic fluid, which limits the fetus’s chances of survival.
The state’s Republican-led legislature is swiftly moving toward passing a far stricter law banning abortion after six weeks of pregnancy. The new measure — which passed the Florida Senate last week and is awaiting final passage in the House — adds exceptions for rape and incest but does not address PPROM.
One of the sponsors of Florida’s 15-week abortion ban defended the current law as written, saying the existing exception should be sufficient to cover cases with serious health risks. An explicit exception for PPROM is not necessary, she added.
“The bottom line is we value life, and we would like to protect life,” said former Florida state senator Kelli Stargel (R). “We don’t want to give a gaping exception that anyone can claim.”
Of all the pregnancy complications affected by abortion bans, pre-viability PPROM is one of the most widespread, according to doctors interviewed for this story. The condition is common enough that one day after Cook was turned away from the hospital, the same thing happened to one of her closest friends. Shanae Smith-Cunningham, 32, was 19 weeks into her pregnancy when her water broke.
This story of what happened to the two friends is based on over 200 pages of medical records provided by the patients and on internal hospital documents, as well as text messages, videos and social media posts. In addition to Cook and Smith-Cunningham, The Washington Post interviewed friends and family members who witnessed the events, and several of the doctors involved in the women’s care.
#Abortion#Reproductive rights#Tw pregnancy loss#Health care#reproductive justice#reproductive rights
42 notes
·
View notes
Text
https://www.washingtonpost.com/politics/2023/04/10/pprom-florida-abortion-ban/
21 notes
·
View notes
Text
Highlights of the internship - Week 7:
• Identifying aortic dissection on CT and the attending being so proud that he talks about it even in the OR. “Do you know what she has recognised today??”
• Had to hold and protect intestines from any possible damage for such a long time that I am glad my spine does not have a new distorted shape now because of my wrong and bad position.
• I could close the half of the subcutaneous tissue and skin on a midline incision simultaneously with a resident, I can feel that I gain speed and it does make me content.
• The fact that all the C-sections I have attended in this week came across with the same doctor feels like I am part of his team now haha.
• I didn’t do surgery like my attending said but I assisted him at one, there was only one nurse so I was more active.
I was melt by his words when I opened the topic of residency during this surgery; “I would love to have you as a resident here and work with you. If you choose this hospital, I will provide you all the opportunities to equip you as best as I can for this job.
“Either way, I know that you will be a known and respected doctor in the OB/GYN community.” 🥹
• During a conversation about some kids’ relationship with their doctor father, a nurse insinuated that I must have chosen medicine because of money after my attending mentioned that my father is doctor too. How all this ended after she was not convinced by me that it is not right was my attending trying to defend me with saying that I chose it because I must have emulated my father’s job. That is right but she didn’t believe.
• While watching an operation which was getting done by some residents, my shoulder has been poked behind my back by my attending. I turned my head only to hear him saying, “look, you are going to be doing these operations if you come here.” Way to steal my heart and mind.
• An OB/GYN doctor has talked to me for about 30 minutes about why I should not choose this specialty. I can see his points about it being really demanding and requiring sacrifice from your social life, etc. However, one point of him was rather disturbing, I don’t even call it a point; at surgery, it is like testosterone in women increases because they lose femininity. Will your husband put up with your testosterone? There will be more femininity at others.”
The way, some of them wants me to plan my life on a non-existent husband 🤦🏻♀️
And I did definitely mentioned about this to my attending, how nobody around ever says OB/GYN is good. “Okay, fine, let’s say it is bad. But you obviously do love bad, you can choose it.
“There has got to be some people who will choose it. If people like you or me don’t it, then who will?”
• Found fetal heart on ultrasound by myself!!
• After my first time doing it at 4th year, I again did curettage for abortion with the same doctor. Memoriesss!!
• I had my first weekend shift of OB/GYN at this week. What are the odds of two women who were pregnant with twins coming in for PPROM at about the same gestation weeks and getting admitted for urgent C/S in the same day? Also to the same doctor of whose C/S operations I have been attending in the previous days? We really are about to become a team haha
#ob/gyn#internship#6th year#medical student#medical stuff#medical school#medblr#night shift memories
2 notes
·
View notes
Text
This post pertains to pregnancy loss
I feel so bad for BFF. Her husband is…well, IMO not the ideal partner although I know she really loves him. He has mental health issues and trauma and in the time they’ve been together he’s gone to mental illness treatment programs twice. He’s sort of been up and down with regards to how much he is working on these issues. I forget the timeline now but I think he was either just out of treatment or like floundering and needing to go back to treatment, near the time of their wedding (like, not RIGHT before, maybe somewhere in the year prior). I told BFF I thought she should postpone her wedding due to these issues, and that went terribly, and I would now advise anyone NOT to say that to someone, esp if the person isn’t asking “do you think I should postpone my wedding?” 🫣 […thinking back on it I think it wasn’t that he was just out of treatment, it’s that he had already been to treatment a while ago and they were repairing trust and then she found out he’d been fired from a job and tried to cover it up, which was the second time he’d done that. Something bad that made me feel justified in saying it! But still]
He hasn’t been to therapy in a while for various reasons, some BS and some not, and then in late September BFF’s pregnancy ended at 18 weeks due to PPROM and it was awful. He still has not been back to therapy since then!
And now they have had two very rough conversations where he is, I think, trying to say that he no longer wants to have a kid. But he is scared of saying that directly cause he knows she still does. And it’s hard to tell how “real” this opinion is, cause he’s saying all kinds of textbook depressed/unprocessed grief stuff, like “I think the world is too messed up to bring a kid into” (as opposed to, say, “I don’t think I can risk going through that pain again”). So BFF is thinking that if he processed his grief and got more treatment for his depression, he’d come back to his original position of wanting kids. Which…maybe! But also maybe not! And so I feel terrible for her and possibly irrationally irritated with him, but also really hoping that if he does want to be done trying, they get that out in the open sooner rather than later so she can figure out what she wants to do!
5 notes
·
View notes
Text
Premature Birth: Signs, Causes, Complications, and Treatment

Premature birth, or preterm birth, is when a baby is born before 37 weeks of pregnancy, whereas a full-term pregnancy lasts around 40 weeks. This early delivery can lead to various health problems, making it crucial for expectant mothers to understand the signs, causes, and treatment options.
What is Premature Birth?
Premature birth happens when delivery occurs before 37 weeks of pregnancy. It is the leading cause of death in children under five and can result in lifelong disabilities. Premature births are categorized based on gestational age:
Extremely Preterm: Born before 28 weeks
Very Preterm: Born between 28 and less than 32 weeks
Moderate to Late Preterm: Born between 32 and 37 weeks
Signs and Symptoms of Premature Birth
Call your doctor immediately if you notice any of these signs before 37 weeks of pregnancy:
Regular Contractions: Tightenings or cramps that come at regular intervals, sharp backache, or persistent pelvic pressure.
Fluid Leakage: Gushing or trickling of fluid from the vagina, especially if the fluid is discoloured.
Vaginal Bleeding: Any bleeding during pregnancy.
Decreased Fetal Movement: A noticeable reduction in your baby’s movements.
Early detection and treatment can help prevent complications and improve outcomes for both mother and baby.
Causes of Premature Birth
Premature birth can occur spontaneously or be medically induced. Common causes include:
Previous premature birth increases the risk.
Placental problems, such as placental abruption or placenta previa.
Abnormal amounts of amniotic fluid.
Preterm premature rupture of membranes (PPROM).
Uterine abnormalities or a short cervix.
Multiple pregnancies (twins, triplets).
Chronic maternal health conditions like high blood pressure or diabetes.
Pregnancy-related conditions such as preeclampsia or gestational diabetes.
Infections and fetal growth restrictions.
Risk Factors
Being very young (under 18) or older (over 40).
Higher incidence in Black women compared to other ethnicities.
Being underweight or overweight before pregnancy.
Smoking, alcohol use, or illicit drug abuse.
High levels of stress or depression.
Diagnosis
Doctors diagnose premature birth through:
Pelvic Assessment: Checking cervix dilation and uterus firmness.
Ultrasound: Measuring cervical length and assessing fetal and placental issues.
Uterine Monitoring: Measuring contraction duration and spacing.
Urine Test: Checking for bacterial presence.
Treatment
For preterm labour or risk of premature birth, treatments may include:
Antenatal Steroids: To help mature the baby’s lungs faster.
Tocolytic Medications: To delay labour temporarily.
Antibiotics: To prevent infections if water breaks early.
After birth, premature babies often need specialized care in the NICU, including:
Incubator Care: To maintain body temperature.
Respiratory Support: Using ventilators or CPAP machines.
Feeding Assistance: Initially through IV or feeding tubes.
Phototherapy: To treat jaundice.
Complications
Premature birth can lead to:
Short-term complications: Breathing problems, heart issues, brain problems, digestive issues, blood problems, metabolism problems, and immune system problems.
Long-Term Complications: Cerebral palsy, learning disabilities, retinopathy of prematurity, hearing loss, enamel defects, and increased risk of conditions like autism spectrum disorder.
When to See a Doctor
Contact your doctor if you experience:
Regular contractions or tightenings.
Excess fluid leakage.
Vaginal bleeding.
Reduced fetal movements.
Persistent pelvic pressure.
Prevention
To reduce the risk of premature birth:
Maintain a Healthy Weight: Through a balanced diet and exercise.
Stay Active: To reduce risks of complications.
Manage Stress and Depression: Seek help if needed.
Quit Smoking and Avoid Alcohol: For a healthier pregnancy.
Check Medication Safety: Ensure medications are safe for pregnancy
Prevent Infections: Practice good hygiene.
Even with no identifiable risk factors, regular prenatal care is essential.
Conclusion
Premature birth is a complex issue with significant implications. Understanding the signs, causes, and potential complications can help expectant parents manage this challenging situation. With advances in medical care, many premature babies lead healthy lives. For comprehensive care, choose the best hospital in Varanasi.
For personalized care and support, visit Arvachin Hospital, a leading medical facility dedicated to providing top-notch healthcare.
0 notes
Text
When reviewing contraceptive options, one should consider how the main pharmacologic ingredient affects the menstrual cycle based on the follicular and luteal phases. Estrogen increases during the follicular phase and culminates in ovulation. Estrogen-containing contraceptives regulate ovulation. Progesterone increases during the luteal phase, causing the proliferation of the endometrial lining and changes in the cervical mucous. Progesterone-containing contraceptives regulate bleeding and mucus production.
If a patient becomes pregnant with an IUD in place and the strings are visible on exam, then removal with gentle traction should be attempted. In general, IUDs should be removed prior to 12 weeks. After this time frame, the risk of miscarriage increases.
When a patient presents prior to 34 weeks with PPROM, expectant management is indicated along with betamethasone, prophylactic antibiotics (ampicillin, amoxicillin, and a macrolide), and magnesium (if prior to 32 weeks). Tocolysis may be considered for up to 48 hours to allow for betamethasone administration. Induction of labor should be performed if there are signs of infection or fetal/maternal instability. For patients who present after 34 weeks, induction of labor should be performed to prevent infections and other adverse outcomes. Gentamicin and ampicillin should be given if there are signs of infection (fever, tachycardia, purulent amniotic fluid).
Complete abortions occur prior to 20 weeks gestation and are characterized by vaginal bleeding/cramping, passage of the products of conception, and a closed cervical os on physical examination.
A missed abortion presents with closed cervical os and fully retained products of conception.
Pituitary adenomas are benign neoplastic proliferations of one or more pituitary cell types. The pituitary contains several different cell types, which secrete their respective hormones. Pituitary adenomas may be functioning or nonfunctioning (so-called "silent"). As such, they may present clinically with symptoms of hormone overproduction or with local mass effects (visual disturbances, headache). They also may be asymptomatic and discovered incidentally on imaging. Silent adenomas are more likely to be larger upon diagnosis.
The most common pituitary adenoma overall is lactotroph adenoma, or "prolactinoma." Prolactinomas are usually clinically apparent in females (with menstrual irregularities or galactorrhea) but may be clinically silent in males. Gonadotroph adenomas are usually nonfunctioning and are more likely to present with mass effects. Thyrotroph, somatotroph, and corticotroph adenomas may be functioning or nonfunctioning. While functioning, thyrotroph adenomas present with signs of hyperthyroidism, somatotroph adenomas present with acromegaly, and corticotrophs present with Cushing-like features.
The workup of a pituitary adenoma is complex due to the various hormones involved. Initial imaging includes a dedicated pituitary MRI, which will reveal a sellar mass. Measurement of the various pituitary hormones or their downstream effects (ie, insulin-like growth factor-1, thyroid hormones) can assist in diagnosing the subtype of pituitary adenoma.
Small prolactinomas are often managed medically with dopamine agonists. Large adenomas and other types of functioning adenomas usually require surgery.
2 notes
·
View notes
Text
Two friends were denied care after Florida banned abortion. One almost died.
When abortion was legal across the country, doctors in all states would typically offer to induce or perform a surgical procedure to end the pregnancy when faced with a pre-viability PPROM case — which is the standard of care, according to the American College of Obstetricians and Gynecologists (ACOG), and an option that many women choose. Especially before the 20-week mark, a fetus is extremely unlikely to survive without any amniotic fluid.
But in the 18 states where abortion is now banned before fetal viability, many hospitals have been turning away pre-viability PPROM patients as doctors and administrators fear the legal risk that could come with terminating even a pregnancy that could jeopardize the mother’s well-being, according to 12 physicians practicing in antiabortion states....
A 2022 study on the impact of Texas’s six-week abortion ban found that 57 percent of pre-viability PPROM patients in Texas who were not given the option to end their pregnancies experienced “a serious maternal morbidity,” such as infection or hemorrhage, compared with 33 percent of PPROM patients who chose to terminate in states without abortion bans. According to 2018 ACOG guidance, “isolated maternal deaths due to infection” have been reported in early PPROM cases....
After everything they’d been through, would either of them ever be able to have a baby?....
The surgery worked for Smith-Cunningham, but not for Cook.
https://www.washingtonpost.com/politics/2023/04/10/pprom-florida-abortion-ban/
0 notes
Text
"Over the course of the day, according to medical records, Cook would lose roughly half the blood in her body.
She had intended to deliverthe fetusin a hospital, a doctor by her side. When her water broke the night before — at least six weeks ahead of when a fetus could survive on its own — she drove straight to the emergency room, where she said the doctor explained that she was experiencing pre-viability preterm prelabor rupture of the membranes (PPROM), which occurs in less than 1 percent of pregnancies. Thecondition can cause significant complications, including infection and hemorrhage, that can threaten the health or life of the mother, according to multiple studies.
At the hospital in Coral Springs, Fla., Cook received antibiotics, records show. Then she was sent home to wait."
---Two friends were denied care after Florida banned abortion. One almost died.
1 note
·
View note
Text
Erken doğum tedavisi, 37. haftadan önce doğum başlama belirtileri olması nedeniyle yapılan tüm tıbbi müdahaleleri kapsar. Erken doğum başladıysa, doktorunuz kasılmalarınızı durdurmanıza ve sizin ve bebeğinizin sağlık problemleri yaşamasını önleyebilecek bazı tedaviler önerebilir.
Erken doğum tedavisi, erken doğumun durdurulması için bir garanti vermez. Ancak erken doğum başladıysa, daha uzun süre hamile kalmanıza yardımcı olabilirler.
Erken doğum tedavisinde hangi ilaçlar kullanılır?
Erken doğum tedavisinde sırasında zaman kazanmak için ağrı kesici işlemi yapılır. Bu sürece uterus kasılmaları denir. Bunun için ritodrin, magnezyum sülfat, nifedipin, indometasin, oksitosin antagonistleri (atosiban), nitrik oksit gibi ilaçlar kullanılabilir. Medikal tedavinin yanı sıra dinlenme, dehidrasyon ve sakinlik önemlidir. 24 ila 34. gebelik haftaları arasında, doğumdan önce akciğerleri tam olarak gelişmemiş olabilecek bebeklere yardımcı olmak için annelere betametazon tipi kortikosteroidler verilir.
Erken doğum tedavisinde doktorunuzun size verebileceği üç tür ilaç vardır:
Doğum
öncesi kortikosteroidler (ACS)
Bu ilaçlar
bebeğinizin akciğer gelişimini hızlandırır. Ayrıca bebeğinizin doğumdan sonra
belirli sağlık sorunları yaşama riskini azaltmaya yardımcı olur. Bunlar
arasında şiddetli dispne sendromu (RDS) adı verilen bir solunum bozukluğu;
intraventriküler kanama (IVH) adı verilen beyinden kanama ve bebeğinizin
bağırsaklarında nekrotik enterokolit (NEC) olarak bilinen bir durum sayılabilir.
Antibiyotikler
Bunlar
bakterilerin neden olduğu enfeksiyonları öldürür. Eğer B Grubu strep
enfeksiyonu geçiriyorsanız veya dönemden önce membranların erken yırtılması
(PPROM olarak da bilinir) varsa, siz ve bebeğinizdeki enfeksiyonları önlemek
için antibiyotiklere ihtiyacınız olabilir.
Tokolitikler
Bunlar doğum
kasılmalarını azaltır veya durdurur. Tokolitikler doğumu geciktirebilir. Tokolitikler
doğumu genellikle sadece birkaç gün geciktirir. Bu gecikme size ACS tedavisine
girmeniz veya yenidoğan yoğun bakım ünitesi olan bir hastaneye gitmeniz için
zaman kazandırabilir.
Erken doğum için diğer tedaviler
Erken doğum tedavisi
Progesteron
Normalde
vücutta bulunan bir hormondur. Progesteron tedavisi geçmişte bir spontan erken
doğum olduysa, prematüre doğumu önlemeye yardımcı olabilir. Progesteron ayrıca
kısa serviks olan kadınlarda erken doğumun önlenmesine yardımcı olabilir.
Serklaj
Erken doğum tedavisinden olan serklaj, doktorun servikse yaptığı bir tür dikiştir. Bu dikiş, serviksin kapalı kalmasına yardımcı olabilir. Böylece bebeğiniz çok erken doğmaz. Doktor, hamileliğin yaklaşık 37. haftasında dikişi çıkarır. Serklaj sadece belirli kadınlar için kullanılır. Örneğin, serviksiniz kısaysa doktorunuz serklaj önerebilir.
Yatak
istirahati
Doktorlar,
yatak istirahatinin erken doğum belirtileri olsa bile hamileliğinizi daha uzun
süre korumanıza yardımcı olup olmadığını tam olarak bilmiyorlar. Dinlenme,
bebeğiniz doğana kadar zorlanmamanız, sakin kalmanız ve hareketsiz kalmanız
gerektiği anlamına gelir. Doktorunuz sizi gün boyunca yalnızca birkaç kez
dinlenmeye yönlendirebilir. Ya da bütün gün yatakta kalmanızı isteyebilir.
Doktor tarafından önerilen yatak istirahati erken doğumun önlenmesine yardımcı
olabilir.
Erken doğum tedavisinde kullanılan ilaçların anne ve bebek için yan etkileri
Erken doğum tedavisi için kullanılan ilaçlar, size veya bebeğinize yardımcı olmak için gerekeni yapabilir, ancak yan etkileri de olabilir. Yan etkiler her kadın için farklı olabilir ve aldığınız ilacın türüne bağlıdır. Sizin için ne tür ilaçların uygun olduğunu öğrenmek için doktorunuzla konuşun.
Antenatal
kortikosteroidler
Erken doğum tedavisinde kullanılan bu ilaçların anne için olası yan etkileri, vücutta sıvı birikmesi ve daha yüksek kan basıncı olabilir. Bebek için hiçbir yan etkisi yoktur.
Tokolitikler
Erken doğum tedavisinde, her biri farklı yan etkilere sahip olan çeşitli tokolitik tipleri vardır.
Terbutalin
gibi beta reseptör adrenerjik agonistleri
Bebeğiniz
için olası yan etkiler arasında hızlı kalp atış hızı olabilir. Sizin için olası
yan etkiler şunlardır:
Göğüs ağrısı hızlı veya düzensiz kalp
atışı
Nefes darlığı; akciğerlerde sıvı
İshal, bulantı (mide rahatsızlığı),
kusma
Baş dönmesi hissi titreme veya
sinirlilik; nöbetler
Ateş, baş ağrısı
Yüksek kan şekeri
Düşük tansiyon; düşük kan potasyumu
Nifedipin
gibi kalsiyum kanal blokerleri
Bebeğiniz için erken doğum tedavisinde kullanılan bu ilacın yan etkisi yoktur. Sizin için olası yan etkiler şunlardır:
Kabızlık, ishal, bulantı
Baş dönmesi veya halsizlik
Baş ağrısı
Düşük tansiyon
Deride kızarıklık
Magnezyum
sülfat
Erken doğum tedavisinde bebeğinizin yan etkileri şunlar olabilir:
Yorgunluk ve uyuşukluk
Daha yavaş nefes alma
Zayıf kaslar
İlaç 5 ila 7 günden fazla
kullanılırsa düşük kalsiyum seviyeleri ve kemik problemleri
Sizin için
yan etkiler şunlardır:
Nefes darlığı, akciğerlerde sıvı
Ağız kuruluğu
Yorgunluk (çok yorgun hissetme),
zayıf kaslar
Baş ağrısı, çift görme, konuşma
problemi
Kalp krizi
Bulantı veya kusma
Cildin kızarıklığı, yoğun terleme
İndometasin
gibi steroidal olmayan anti-enflamatuar ilaçlar (NSAID'ler)
Bebeğinize
yan etkileri şunlar olabilir:
Beyinde veya kalbinde kanama
Patent duktus arteriozus (PDA).
Prematüre bebeklerde sık görülen bir kalp problemidir.
Sarılık
Çok az idrar yapmak gibi böbrek
problemleri
Nekrotik enterokolit (NEC). Bebeğin
bağırsaklarında bir sorundur.
Akciğerlerde artmış kan basıncı
Sizin için yan
etkiler şunlar olabilir:
Baş dönmesi
Mide ekşimesi
Bulantı veya kusma
Oligohidramnios
İltihaplı mide astarı
Vajinal kanama
0 notes
Text
It was the first week that Anya Cook, 36, felt comfortable going out as a fully fledged pregnant person. She was well into her second trimester – 16 weeks – but having suffered 17 miscarriages in two years, she had learned not to get hopeful too early. In December 2022, her city of Coral Springs, Florida, was having its annual parade. Cook felt cute in her two-piece biker-short set as she watched children stuff their faces with ice creams, while parents cheered on the marching band from the sidelines.
Leaving a restaurant later that evening, Cook felt a wet rush down her legs, like someone had thrown a glass of water on her. On the way to the hospital with her husband, Derick, she hoped that even if her water had broken, she could get a small stitch and continue with a healthy pregnancy.
When Cook got to the ER, as far as she could see, no one had been shot, or was in need of urgent care. But over the next hour, she would learn how it felt to be invisible. The receptionist told Cook no beds were available, although Cook believes she saw many sitting empty. People turned their heads away as Cook squirmed uncomfortably in a wheelchair, amniotic fluid gushing between her legs. “Mommy, what happened to her?” she heard a small boy visiting the ER ask. The boy’s mother shushed him.
Soon, Cook would find out. Her water had indeed broken early, and there was no stitch that could reverse it. In the next 48 hours, she would deliver and her fetus would not survive.
Cook would be sent home, to deliver on her own. Because the doctors could still see a fetal heartbeat on the ultrasound, she couldn’t have an abortion, even though they knew 16 weeks was too early for it to survive. And because Cook was not yet in a life-threatening situation, the doctors couldn’t intervene to save her.
“I said, ‘Let me guess. Is it because of Roe v Wade’?” says Cook by phone interview.
The doctor confirmed it was.
Cook left the hospital certain of her fate that evening. After scouring the internet to learn about PPROM – preterm premature rupture of the membranes – she was sure she was going to die: complications from PPROM can include serious infection and hemorrhage.
Cook booked an appointment at the salon the next morning to have her hair done, ready for her casket. She and Derick argued all the way there. He couldn’t believe she was giving up.
Cook delivered her daughter, who she named Bunny, a few hours later, in the salon toilet. In the small, sterile-smelling room, she sat on the toilet with Derick between her legs, and tried to direct him, telling him to remove the cord and help her deliver her placenta, based on things she had seen on TV.
One of the clients in the salon that day was a nurse. When she saw Cook, she spoke with urgency: Cook was hemorrhaging and needed to get to the hospital, stat.
Cook remembers feeling dismissed and questioned when she arrived at the hospital. “The paramedics told them I was bleeding out,” says Cook. Still, she says she was asked by nurses and doctors several times if she was OK before being rushed for treatment.
In the end, to be taken seriously, Cook says she opened her legs. “I literally just released my body and blood. Like a pipe that burst in your kitchen, blood – gushing, shooting out,” explains Cook. “I said, now do you believe me?”
She woke up the next day, having lost almost half of the blood in her body. Lasting damage to the blood vessels around her uterus may make it even harder for her to get pregnant again.
Asked if she believes race was a factor in her care, Cook says yes.
“If I was Ron DeSantis’s wife, I would have gotten the care I needed, right there in that very moment,” she said – referring to the night when she first arrived in the ER.
Forced birthers, please explain to me why you don't deserve to have this happen to you. Because whenever someone tells you you should go through this, you cunts clutch your pearls.
"How could you wish that on anyone, you cretin!?!" You say.
You force unimaginable pain on others but you get all pissy at the idea of it happening to you. Well, I think you need it to happen to you. You're incapable of empathy, so the only possibility that you'll feel the least bit sorry for what you've done is when you're on the floor, begging doctors to help because it's different when it's you.
2 notes
·
View notes
Photo

Another throwback! One that is no longer painful or angering, I’ve even forgiven myself. It’s more like an “oh man look what we survived, we really did that and are still here..woah” 6 years ago February I was hospitalized and on complete bedrest for a little over a month. He spent 2 weeks in the nicu. I didn’t think he was gonna make it, but if I could go back I’d tell myself while I was laid up in that bed don’t stress too hard. Listen to all your amazing friends and family that dropped by to give love an encouragement. He IS gonna be tearing everything up, active and love the outdoors, in no time. All that stress for different stress 😂 now it’s more like how do I keep this kid from leaping out of trees and sliding off trails💀. Makoa is definitely a #pprom baby that continues to thrive. He’s finally on the charts in weight, low, but ok!! He’s tall for his age apparently, idk anything about height, I stopped growing at age 8🤷🏽♀️ his hair is to his knees💪🏽 and he constantly burns thru notebooks and notepads because he LOVES to draw and/or paint. Obsessed with jaws and Jurassic park, he can play bits of the theme songs on the piano! Favorite food is rice, eggs and spam, fav color is Red. He can tell never ending, GRAND stories, his mind is incredibly vivid. Just a wild and crazy guy that sometimes I don’t know what to do with!!!🙏🏽 #tbt #34weeker #preemiestrong #makoakai_ (at Glendale Adventist Hospital) https://www.instagram.com/p/CLc54A4n_6-/?igshid=5d6ivcz72wuf
6 notes
·
View notes
Text
What BFF had is called pPROM (preterm premature rupture of membranes). I saw her today and she said she made the mistake of googling more about it and found all these “PPROM at 18 weeks and now my baby is happy and healthy!” stories. How horrible. I have now looked (just googled “PPROM 18 weeks”) and so many of those blog posts are in the top results. That’s gotta be like…anti choice propaganda, right? Her doctor told her that of the babies who survive the wait until they’re old enough for labor to be induced, and then the NICU, only 3% go home without catastrophic health problems. But that’s not necessarily the impression I’m getting from cursory googling. Ugh.
This has all been really interesting, like…psychologically. I weirdly happened to be digging into An Exact Replica of A Figment of My Imagination (Elizabeth McCracken’s memoir about having a stillbirth while living abroad in France) right as BFF found out what was happening. You might think I’d have then set it aside because the synergy is too sad, but it’s actually been really helpful. I did briefly think “did I somehow cause this by reading this book” which of course is bizarre. So many things BFF has been saying are direct echos of what I’m reading here (like “if I get pregnant again I won’t tell anyone until I have the baby”). I was at lunch with some other friends and told them about the situation, and one of them who I really like and who has had one miscarriage of her own at maybe 12 weeks, said something like “I just think, about my own miscarriage, thank god - because [something about how something must have been wrong with the baby]” so I just politely said “okay yes that makes sense but just so you know, nothing was wrong with BFF’s baby, they’d just gotten extensive genetic testing results back” …it’s interesting how the urge is SO STRONG to put a “this makes sense” or “it might even be a silver lining” bow on it. BFF just keeps repeating what one of her doctors said to her - “this is just a shitty thing that happened”…blunt but oddly comforting?
Idk there’s no end to the thought here, I’m just continuing to think a lot.
5 notes
·
View notes